Using the strength of the human immune system, a team of engineers at the University of California, San Diego, has created a biodegradable polymer system to treat rheumatoid arthritis, an autoimmune and inflammatory disease.
The study builds on earlier work with all-trans retinoic acid (ATRA), which is produced naturally in the body and aids in cell growth and development, and on the growing clinical interest in immune system modulation as a cancer and autoimmune disease treatment. The team adds two significant innovations to earlier approaches by approaching these problems from the perspective of a biomaterials engineering lab: local release and utilizing the shared microenvironment for long-lasting effectiveness.
This procedure involves injecting encapsulated ATRA directly into a rheumatoid arthritis-affected joint, where it acts for at least a few weeks. This is when regulatory T cells, which are capable of treating or preventing the disease elsewhere in the body, are created when ATRA converts disease-causing cells into disease-stopping cells.
“Our method essentially converts the disease location into a factory that creates regulatory T cells. It employs a biodegradable biomaterial to enable the controlled release of ATRA, which reprograms T cells to cure illness.”
David A. McBride, a chemical engineering graduate student at UC San Diego.
In essence, according to David A., “our system converts the disease site into a factory that generates regulatory T cells.”. Nisarg Shah, a professor of nanoengineering at UC San Diego, is McBride’s graduate advisor in chemical engineering. “It uses a biodegradable biomaterial to enable the timed release of ATRA, which rewires T cells to treat disease.”.
The study was released in the journal Advanced Science. The paper includes McBride as a co-author.
Iannis Adamopoulous, an associate professor of medicine at Harvard’s Beth Israel Deaconess Medical Center’s Department of Medicine, Division of Rheumatology, said that this is a very promising line of research that uses the most cutting-edge immunoengineering technology to combat arthritis.
Describe ATRA.
The FDA has currently approved the small molecule ATRA for the treatment of acute promyelocytic leukemia (APML). It may also be effective in treating autoimmune arthritis and reducing inflammation, according to 20 years of research. However, that approach depends on ATRA dispersing unchecked throughout the body, which can lead to immunosuppression, significant off-target toxicity, and other negative side effects.
The potential of ATRA to treat autoimmune arthritis was previously demonstrated, but McBride claimed that the route of administration prevented clinical application of the research.
ATRA can be injected directly into joints when it is enclosed in biodegradable materials at therapeutic concentrations, but as it diffuses out of the joint, it enters the circulation at much lower concentrations, reducing or eliminating side effects. Patients would need multiple injections per day to achieve the same effects without the controlled release made possible by the biomaterial encapsulation, which is frequently not practical.
How it functions
Helper T cells scour the body for disease-causing pathogens when the immune system of humans is functioning properly. A helper T cell can enlist additional cells to assist in the fight against a pathogen when it is found. In a way, McBride said, “It’s like having police cars driving around the city, and when one sees a crime happening, they call for backup to get things under control.”.
Numerous autoimmune diseases are caused by instances of “mistaken identity,” in which these cells attack a perceived threat target that is actually a component of the body’s normally functioning cells. Such pathogenic T cells, which McBride refers to as “bad apples,” can proliferate in the body as a result of a combination of genetic and environmental factors. When they summon large teams of immune cells for pointless standoffs, these pathogenic T cells can cause havoc on the body.
For instance, according to McBride, “in type 1 diabetes, you have bad apples that call in reinforcements against your pancreas.”. It works against your neurons in multiple sclerosis. It works against your joints in rheumatoid arthritis. Your immune system then recognizes this as a target for attack and sends a ton of extra immune cells to these areas to wage war until all the pathogens are eliminated. In this instance, however, the healthy parts of the body are being attacked rather than pathogens.
Numerous current methods obstruct the chemical signals immune cells use to communicate, effectively stopping pathogenic T cells from recruiting support without getting rid of the “bad apples.”. Time-released ATRA rewires them to function as regulatory T cells, or “good apples. These cells still have the capacity to detect and respond to immune cell activity in the joints, but instead of mobilizing more immune cells, they work to reduce inflammation. The sustained-release formulation enables adequate therapeutic exposure to tip the scales in places like joints, which are not advised for repeated injections.
The anti-inflammatory regulatory T cells perform better thanks to long-lasting changes made by ATRA to the cellular machinery’s capacity to read cell DNA. In doing so, regulatory T cells are produced that are particular to the diseased tissue and are used to treat T cells at the disease site. Then, when these cells are transferred to other disease sites, they can assist in reducing inflammation and encouraging healing. The cells’ disease-specificity prevents them from interfering with healthy immune function, allowing them to supplement currently available treatments or offer patients who require them alternatives.
“The coolest thing about this is that the treated site of disease, where the bad apples were previously proliferating, now becomes a place that can generate regulators,” said McBride. “These regulators can patrol the body and actually prevent disease.
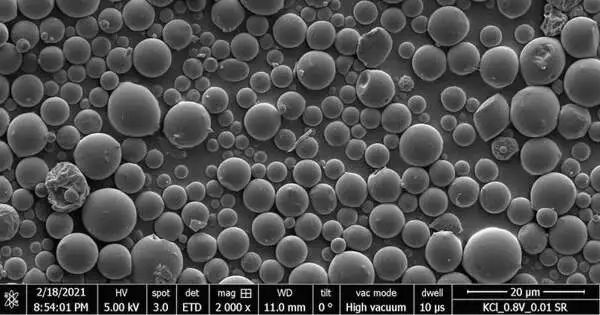
David McBride, a student at UC San Diego studying chemical engineering, creates a biodegradable polymer system that may one day be used to treat rheumatoid arthritis. David Baillot/Jacobs School of Engineering, UC San Diego
the limitations of current methods.
Disease-modifying anti-rheumatic drugs (DMARDs) are commonly used to treat patients with rheumatoid arthritis, and for many of them, this strategy is effective. Front-line DMARDs have some significant drawbacks and adequately treat about one-third of patients.
First off, some patients who use DMARDs experience weakened immune responses to vaccines and increased susceptibility to infectious disease. This is because, according to McBride, “the COVID-19 pandemic has brought a lot more understanding of the risks of immunosuppression into public awareness.”.
Additionally, there is no way to stop treatment if a risky infection develops because the majority of immunosuppressive medications used to treat rheumatoid arthritis remain in the body for up to two weeks. When patients use two or more treatments at once, which is common given the complexity of the disease, this is made worse. The risks of infections or cancer can be increased by taking several potent immunosuppressants.
“If you can have a treatment option that doesn’t have an immunosuppressive effect, you can really reduce the risk for patients who need multiple treatment modalities to keep their autoimmune disease in check,” McBride said.
Lastly, immunosuppressive medications for some patients may initially be effective before losing that effectiveness. When new disease pathways or antibodies that neutralize the drugs are produced by their bodies, this can occur. This and other new therapies may be used in conjunction with DMARDs to make up for declining efficacy or to start with lower doses.
“In well-controlled patients, reducing or eliminating the need for immunosuppressive medications is desirable,” said Shah. However, research has shown that the disease can flare up again when it is attempted. Therefore, having a non-immunosuppressive option could be very helpful.
Research strategies, difficulties, and future steps.
The group used a mixture of mouse and human cells to test its biomaterial-encapsulation technique. In order to simulate the remarkable complexity of a real-life case of autoimmune disease in a human subject, they moved from human models of autoimmune arthritis to mouse models after this produced encouraging results.
The work required meticulously tracking the cells from their injection sites to the other locations where they circulated and proved effective in fighting disease, as well as multiple disease models, each created to illustrate a particular aspect of the team’s hypothesis.
To date, the researchers have made significant progress toward commercialization. We currently aim for approval to start clinical trials within five years, but since this is my first encounter with something similar, it is difficult for me to estimate. McBride has taken part in the NSF I-Corps, MedTech Accelerator, and UC San Diego Institute for the Global Entrepreneur (IGE) programs to assess potential commercialization avenues.
More information: David A. McBride et al, Immunomodulatory Microparticles Epigenetically Modulate T Cells and Systemically Ameliorate Autoimmune Arthritis, Advanced Science (2023). DOI: 10.1002/advs.202202720