In collaboration with colleagues in France, researchers at the University of Gothenburg have developed a method that successfully kills the aggressive brain tumor glioblastoma. The cancer dies from stress as a result of a docked molecule blocking certain cell functions.
Disease cells, particularly those that structure forceful growths, are somehow wild and carry on with an exceptionally distressing reality. Cancer cells hijack mechanisms that healthy cells use to regulate protein production and process the excess proteins they produce in order to manage this stress. The cancer cell would die if these hijacked mechanisms continued.
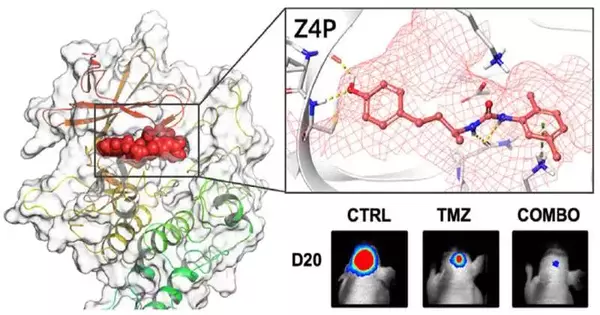
“We have now prevailed with regards to halting this seizing by embedding an exceptionally evolved particle in the cells that hinders one of these captured versatile components in the disease cells. According to Leif Eriksson, a professor of physical chemistry at the University of Gothenburg, this causes the cancer to self-destruct.
“By inserting a specially developed molecule that inhibits one of these hijacked adaptive mechanisms in the cancer cells, we have now succeeded in stopping this hijacking. The cancer self-destructs as a result of this.”
Leif Eriksson, professor of physical chemistry at the University of Gothenburg.
Collaboration between Sweden and France
Leif Eriksson’s team has collaborated with a research team at INSERM in Rennes, France. Utilizing super PCs and high level recreations, the specialists fostered a variant of the particle that can likewise go through the blood-mind boundary that safeguards cerebrum tissue. Their findings have been published in the journal iScience.
The development is applicable to glioblastoma tumors in the brain. These make up around 45% of all mind cancers and around 400 Swedes are determined to have glioblastomas consistently. Each year, there are 19,000 cases across the entire EU. The prognosis for malignant glioblastomas is currently very poor. Five years after diagnosis and treatment, only a small percentage survive.
“Today, malignant growth therapy comprises of a medical procedure, radiation and chemotherapy. Sadly, all disease cells are not killed and the growth returns. When the malignant growth backslide, the cancer cells have frequently spread and created opposition,” Leif Eriksson.
Concentrating on how it very well may be utilized with different tumors
Studies with the new technique have shown exceptionally encouraging outcomes. The researchers discovered that the new drug and chemotherapy alone were sufficient to eradicate the tumors completely and prevent relapse. All cancer cells vanished from the tumors after they were stressed to death, and after 200 days of experiments with mice, there was no cancer recurrence. The brain tumors grew rapidly and relapsed after 100 days in comparative experiments using only chemotherapy.
“These are the first clear results with brain tumors that have the potential to lead to a treatment that completely avoids surgery and radiation.” According to Eriksson, “We have also begun investigating the application of our substance to other aggressive tumor forms like pancreatic cancer, triple-negative breast cancer, and certain lever cancers.”
Different from glioblastomas, there are other kinds of brain tumors that develop differently. With these types of cancer, this new method fails.
No secondary effects
Current medicines for mind growths frequently make extreme side impacts. The substance has not yet had any adverse effects with this new treatment, according to the researchers. The treated creatures kept up with weight, had no clear changes in conduct and there was no indication of effect on the liver. Even at extremely high doses, extensive cell tests have demonstrated that the substance is safe for healthy cells, despite the need for more in-depth research.
The study of this molecule will now proceed. There is still a lot to be done, like making the treatment process work better and doing more experiments on animals. Yet, Leif Eriksson trusts and accepts that it ought to go somewhat rapidly to seek the drug into clinical treatment.
“It largely depends on whether funding is available to enable the various steps to be taken as smoothly as possible. It might take five years, if I’m optimistic. That’s a short amount of time, but glioblastomas are nearly always fatal, so any improvement in medical care is significant, according to Eriksson.
More information: Diana Pelizzari-Raymundo et al, A novel IRE1 kinase inhibitor for adjuvant glioblastoma treatment, iScience (2023). DOI: 10.1016/j.isci.2023.106687