Medication has progressed decisively during the last 100 years. Yet, with regards to getting biopsy results, very little has changed. Consider, for instance, what happens when a patient comes in to have a skin sore biopsied for nonmelanoma skin disease.
“The specialist will take a little piece of the skin out,” says Michael Giacomelli, an associate teacher of biomedical design and of optics at the College of Rochester. Then, “somebody in pathology will check it out under a magnifying lens. And afterward, contingent upon what they find, the patient is informed that “all is great, don’t stress over it, or we want you to return briefly to our arrangement so we can treat you.”
Giacomelli, who is likewise on the examination staff at the college’s Wilmot Disease Foundation, is fostering a clever imaging framework, contained on a compact truck, to abbreviate this cycle to two minutes. This would empower a specialist to quickly decide if the injury is harmful and, assuming this is the case, to “treat the patient during a similar visit as opposed to extending it throughout the following month and various visits.”
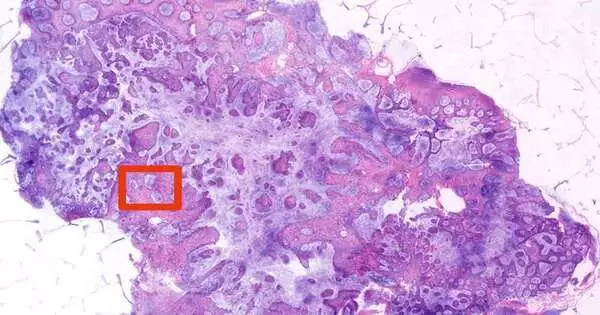
The framework—utilizing two-photon fluorescence microscopy (TPFM)—showed striking precision in a pilot study summed up as of late in JAMA Dermatology. When tried on 15 biopsies of known nonmelanoma skin diseases, the innovation had the option to identify basal cell carcinoma with amazing exactness (100 percent awareness and explicitness) and squamous cell carcinoma with high precision (89% responsiveness and 100 percent particularity).
“The goal is to see how well the technique works in a real-world scenario with a large number of people and a variety of variables. We really want to make sure that there isn’t some strange item that has nothing to do with cancer that we mistake for cancer—or something that does have anything to do with cancer that we can’t imagine. When you start conducting random biopsies on people, you never know what you’re going to uncover.”
Michael Giacomelli, an assistant professor of biomedical engineering and of optics
Nonmelanoma skin disease is the most well-known kind of human malignant growth, with more cases yearly than any remaining sort of disease in the US. A lot of nonmelanoma skin tumors are basal cell carcinomas.
Applications in “a wide range of situations”
Normally, biopsied tissue is extracted, fixed, paraffinized (saved), stained, and mounted on slides prior to being assessed by a dermatopathologist. “Things have been done like this since the late nineteenth century,” Giacomelli says. “A great many biopsies have been done along these lines. Everyone is in total agreement; it works perfectly. The issue is that it is slow. “
In any event, when tissue is immediately frozen for faster examination, specialists can sit tight for an hour or something else for the biopsy results to be certain they have totally taken out a harmful growth from a patient still on the surgical table. This ties up the specialist’s time and the working room, while intruding on the work process in occupied pathology offices.
Giacomelli sees likely applications for his framework in rapidly giving biopsy results to a wide range of illnesses. “There is a wide range of situations,” he says.
For instance, “in prostate cases, specialists frequently have an unfortunate idea of what they’re getting into in view of only an X-beam or X-ray picture in advance,” Giacomelli says. “You see irregular situations where they take out the prostate, and now and again there’s an undeniable cancer that has spread past the prostate, or at different times it is extremely limited. This innovation offers a likelihood to change the patient’s treatment on the fly. “
The upside of utilizing TPFM is that it creates high-goal pictures as well as uses close infrared light that penetrates further through tissue, making it “favorable for fast imaging of new, sporadically molded biopsies with negligible planning,” the paper notes.
Giacomelli is currently working intimately with Sherrif Ibrahim, an academic partner in dermatology at the College’s Clinical Center, on a bigger, 200-patient subsequent review, utilizing biopsy tests taken aimlessly at Ibrahim’s Rochester Dermatological Medical Procedure in neighboring Victor, New York.
“The objective is to dissect the way that well the method works in a true situation, where you have a ton of individuals coming in and a wide range of things can appear,” Giacomelli says. “We truly need to ensure that there isn’t some odd thing that doesn’t regularly have anything to do with disease that we some way or another mistake for malignant growth—or something that has something to do with disease yet we can’t picture. No one can tell you what you will find once you begin taking irregular biopsies of individuals. “
Utilizing TPFM imaging to direct medical procedures?
Giacomelli has also left on the same report to see if a clever framework he created combining TPFM and video can be used to direct medical procedures.
The framework overlays TPFM pictures of the website where tissue is being taken out on a webcam picture, co-enlisting what it resembles to the eye with what it would resemble handled on a slide. “You can show what the extracted tissue resembles, and the amount of the growth is dependent on the extraction,” Giacomelli says. “They can then plan that back into the injury that they are making to conclude which side to cut.”
Notwithstanding Ibrahim, different coauthors of the JAMA Dermatology review incorporate Vincent Ching-Roa and Chi Huang, graduate understudies in Giacomelli’s lab, and Bruce Smoller, teacher of pathology and lab medication.
More information: Vincent D. Ching-Roa et al, Real-time Analysis of Skin Biopsy Specimens With 2-Photon Fluorescence Microscopy, JAMA Dermatology (2022). DOI: 10.1001/jamadermatol.2022.3628
Journal information: JAMA Dermatology