Uppsala University researchers have developed a strategy for killing cancer cells by assisting immune cells to enter a tumor from blood vessels. The objective is to improve how aggressive brain tumors are treated. The study was published in the Cancer Cell journal.
Glioblastoma is a forceful cerebrum growth that needs effective treatment. This is to some extent because of the capacity of the growth to smother or dodge the body’s regular enemy of disease-safe reactions. Immunotherapy, utilizing designated spot inhibitors, can reactivate the resistant framework against disease. Nonetheless, for this kind of treatment to be successful, explicit safe cells known as executioner immune system microorganisms should be available inside the cancer.
Sadly, veins in malignant growth in the cerebrum are useless and go about as an obstruction, keeping executioner lymphocytes from arriving at the cancer. Consequently, although this type of immunotherapy is effective against a variety of cancers, it is ineffective against brain cancers.
“It’s exciting that TLS are formed when we use AAV-LIGHT therapy because killer T cells are thought to be activated against tumor cells in these structures. In our experimental models, we also discovered that the treatment increased survival and, in some cases, was curative.”
Researcher Mohanraj Ramachandran
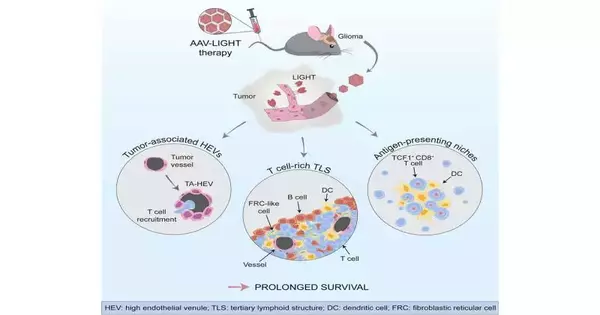
In the new study, the Uppsala researchers have come up with a strategy to make it easier for the killer T cells to get to the tumors and fight cancer cells. They produced a factor known as light by employing a viral vector that specifically infected the brain’s blood vessels. This modified the capability of the cancer vessels, expanding their capacity to ship immune system microorganisms from the blood into the growth tissue.
“We found that the growth veins changed their shape and capability when we involved the viral vector AAV-LIGHT as a treatment in our exploratory glioblastoma models. The blood vessels produce light as a result of the viral vector, which adjusts their function to recruit killer T cells into the tumor. ” Professor Anna Dimberg, who led the study with Professor Magnus Essand, also says that this helps support killer T cell function around the blood vessels.”
Along with the brain tumor, AAV-LIGHT also caused immune cell aggregates known as tertiary lymphoid structures (TLS) to form. These structures have been linked to an increased sensitivity to cancer immunotherapy because they resemble lymph nodes and are found in tumors.
“Because it is believed that killer T cells can be activated against the tumor cells in these structures, it is exciting that TLS are formed when we use AAV-LIGHT therapy. Mohanraj Ramachandran, who collaborates with doctoral students Alessandra Vaccaro and Tiarne van de Walle as the study’s first author, says, “We also found that the treatment prolonged survival and, in some cases, was curative.”
Additionally, the researchers discovered that AAV-LIGHT therapy skewed the TLS composition to include a lot of T cells.
“We were fascinated to figure out that we could control the TLS arrangement for our potential benefit by utilizing our treatment. This is new information that could be utilized as a device to modify the capability of these designs in numerous settings,” says Vaccaro.
“Stem-like T cells,” a subset of killer T cells that resided both within the TLS and in specialized niches around the tumor’s blood vessels, were promoted by the new treatment.
“Because stem-like T cells are known to enhance the effects of immunotherapy, we were thrilled to discover that AAV-LIGHT treatment increased the presence of these cells. According to Tiarne van de Walle, “the significance of the interaction between the various effects of AAV-LIGHT is revealed by finding them within TLS and niches.”
In order to determine whether or not AAV-LIGHT can be utilized for glioblastoma patients, the researchers now intend to further develop this novel treatment.
“While the results are very promising, the viral vector needs more development before we can begin clinical studies. We trust that this new treatment will open up opportunities for patients with glioblastoma later on,” says Essand.
More information: Mohanraj Ramachandran et al, Tailoring vascular phenotype through AAV therapy promotes anti-tumor immunity in glioma, Cancer Cell (2023). DOI: 10.1016/j.ccell.2023.04.010