According to recent research reported in the Journal of Alzheimer’s Disease Reports, SARS-CoV-2 infection has a significant effect on cognitive function in patients with pre-existing dementia. Following SARS-CoV-2 infection, patients with all subtypes of dementia who were a part of the study experienced dementia that rapidly progressed.
Since the initial COVID-19 outbreak, neurologists have observed both short- and long-term neurological syndromes as well as neuropsychiatric aftereffects. Neurologists have referred to “brain fog” as a possible explanation for the effects of COVID-19 on human cognition. “.
The effects of COVID-19 on cognitive impairment in 14 patients with preexisting dementia (four with Alzheimer’s disease [AD], five with vascular dementia, three with Parkinson’s disease dementia, and two with the behavioral variant of frontotemporal dementia) who had experienced further cognitive decline after COVID-19 were studied by a team of researchers driven to better understand and clear up this fog.
“As the world’s population ages and dementia rates rise, we believe pattern identification of COVID-19-associated cognitive deficits is critical for distinguishing COVID-19-associated cognitive impairments from other kinds of dementia. This knowledge will have a significant influence on future dementia research.”
Dr. Souvik Dubey
The principal researchers were Julián Benito-León, MD, Ph.D. and Souvik Dubey, MD, DM, both of the Bangur Institute of Neurosciences (BIN), Kolkata, West Bengal, India. D. , from the Department of Neurology at University Hospital “12 de Octubre,” Madrid, Spain, explained, “We extrapolated our understanding from the cognitive impact of this viral infection in patients without dementia and speculated there must have been some deleterious effect of COVID-19 in patients with preexisting dementia. The evaluation of cognitive impairments in patients with pre-existing dementia after COVID-19 is challenging, though, because of the numerous confounders and biases. “.
The team of researchers discovered that the distinction between various types of dementia became remarkably hazy after COVID-19 in addition to discovering that all subtypes of dementia, regardless of patients’ prior types of dementia, behaved like rapidly progressive dementia after that event.
Ritwik Ghosh, MD, a co-investigator, expressed his concern regarding dementia subtyping at the Burdwan Medical College and Hospital in Burdwan, West Bengal, India. “In the post-COVID-19 era, where the past of this viral infection plays the most significant role, it is more challenging. Few patients with a history of COVID-19 who do not already have dementia exhibit phenotypically and imagingly similar brain changes that mimic other vascular and degenerative dementias. “.
Researchers discovered that after COVID-19, a specific type of dementia’s characteristics changed, and both vascular and degenerative dementias began acting like mixed dementias both clinically and radiologically. Patients with insidious onset, slowly progressing dementia and those who had previously been cognitively stable showed a rapid and aggressive course of decline.
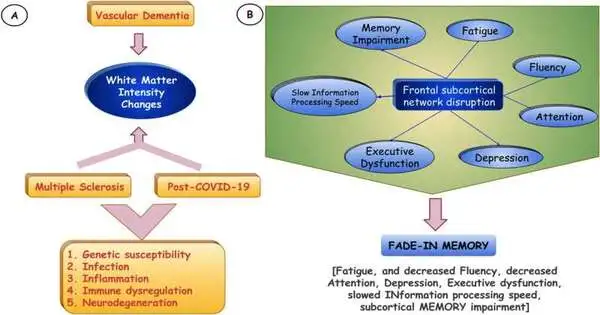
Further follow-ups of the study revealed cortical atrophy to be present. The most significant pathogenetic indicator was thought to be coagulopathy, which involved small vessels and inflammation and was further linked to changes in the brain’s white matter intensity.
The rapid progression of dementia, the addition of new cognitive impairments or declines, and the growth or new emergence of white matter lesions suggest that previously compromised brains have little defense to withstand a new insult (i.e. e. , a “second hit” such as an infection or an inflammatory condition).
“Brain fog” is an ambiguous term that isn’t specifically assigned to the range of post-COVID-19 cognitive sequelae, according to Dr. Dot Dubey and his co-investigators. We suggest a new term, “FADE-IN MEMORY,” based on the progression of cognitive deficits and their correlation with changes in white matter intensity. e. , Subcortical MEMORY Impairment, Fatigue, Reduced Fluency, Attention Deficit, Depression, Executive Dysfunction, Slowed INformation Processing Speed). “.
Among the many psychosocial effects of COVID-19, co-investigator Mahua Jana Dubey, MD, Department of Psychiatry, Berhampur Mental Hospital, Berhampur, West Bengal, India, added, “Cognitive deficits, when accompanied by depression and/or apathy and fatigue in patients with or without preexisting dementia, require meticulous evaluation because it imposes additional stress and burden on caregivers, one of the most significant but frequently overlooked issues that may have the. “.
“Since dementia and the aging population are both on the rise globally, pattern recognition of COVID-19-associated cognitive deficits is urgently required to distinguish between COVID-19-associated cognitive impairments per se and other types of dementia. Future research into dementia will undoubtedly benefit from this understanding, said Dr. Souvik Dubey.
“Increasing epidemiological evidence points to a shared pathogenesis between AD and COVID-19, as shown by the increased risk of AD with COVID-19 and the increased COVID-19 in AD patients. Dubey et al.’s demonstration that COVID-19 fundamentally alters the course of dementia regardless of the cause further demonstrates this connection, according to George Perry, Ph. D. editor-in-chief of the Journal of Alzheimer’s Disease and holder of the University of Texas at San Antonio’s Semmes Distinguished University Chair in Neurobiology.
More information: Souvik Dubey et al, The Effects of SARS-CoV-2 Infection on the Cognitive Functioning of Patients with Pre-Existing Dementia, Journal of Alzheimer’s Disease Reports (2023). DOI: 10.3233/ADR-220090