Specialists at the Lieber Foundation for Mental health (LIBD) accept they have settled an enigma that has tested researchers for over 70 years: how the mind compound dopamine connects with schizophrenia, the frequently wrecking cerebrum issue portrayed by silly reasoning, fantasies and different types of psychosis.
Through their investigation of the outflow of qualities in the caudate core — a locale of the mind connected to profound direction — the scientists found actual proof that neuronal cells can’t exactly control levels of dopamine, and they likewise recognized the hereditary system that controls the dopamine stream. Their discoveries were distributed today in the diary Nature Neuroscience.
“Up to this point, researchers have been not able to unravel whether the dopamine connect was a causative element or exclusively a method for treating schizophrenia,” said Daniel R. Weinberger, M.D., CEO and head of the Lieber Foundation and a co-creator of the review. “We have the main proof that dopamine is a causative figure schizophrenia.”
“Until now, experts had been unable to determine whether the dopamine relationship was a causal element or merely a method of treatment for schizophrenia.”
Daniel R. Weinberger, M.D., chief executive and director of the Lieber Institutec
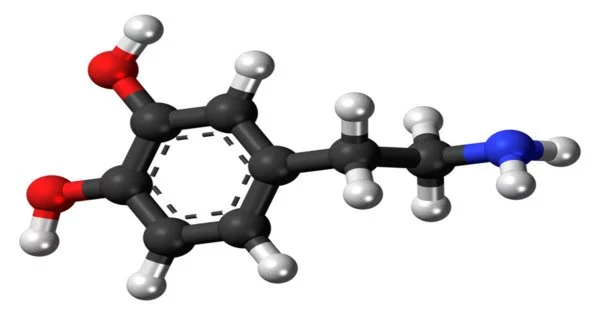
Dopamine, a kind of synapse, goes about as a compound courier that conveys messages between neurons — nerve cells in the mind — to change their action and conduct. Dopamine is the prize synapse that empowers individuals to feel joy.
As per the Public Foundation of Emotional wellness, schizophrenia is 1 of the main 15 driving reasons for handicap around the world, with crazy side effects like fantasies, dreams and confused thinking, as well as decreased articulation of feelings, diminished inspiration to achieve objectives, trouble in friendly connections, engine weakness and mental impedance.
Side effects normally start in late youth or early adulthood, albeit mental weakness and strange ways of behaving at times show up in adolescence. Current medicines for schizophrenia incorporate antipsychotic drugs which address the side effects of pyschosis, yet not the reason.
“One of the significant results of the medications used to treat schizophrenia is absence of joy and bliss,” said Dr. Jennifer Erwin, an agent at the Foundation and one of the creators on the report. “In principle, in the event that we could focus on the dopamine receptor explicitly with drugs, that could be another system for treatment that wouldn’t restrict a patient’s bliss so much.”
Researchers have known for quite a long time that sporadic degrees of dopamine have an association with psychosis and are a basic figure schizophrenia, Alzheimer’s illness and other neuropsychiatric issues. Drugs that increment dopamine in the mind, like amphetamines, are known to cause psychosis. Drugs that treat psychosis do as such by lessening dopamine action.
These perceptions have roused ages of researchers to attempt to grasp whether — and how — an unevenness of dopamine really connects with schizophrenia. Dopamine sends data in the mind by connecting with proteins on the outer layer of synapses, called dopamine receptors. By concentrating on those receptors, researchers at the Lieber Foundation have concocted novel proof affirming that dopamine is a causative element for schizophrenia.
The agents analyzed many posthumous example minds gave to the Lieber Foundation from north of 350 people, some with schizophrenia and others without mental ailment.
They decided to zero in on the caudate core, a piece of the mind that is basically significant for figuring out how to make complex thoughts and ways of behaving more programmed and natural, yet in addition since it has the cerebrum’s most extravagant stock of dopamine. They likewise concentrated on a locale of the human genome that huge global hereditary examinations have recognized as being associated with the gamble of schizophrenia.
This area contains the qualities for the protein receptors that answer dopamine, which focuses to the dopamine-schizophrenia association. Yet, while hereditary information propose all things considered a job of dopamine receptors in danger for schizophrenia, the information are not decisive and don’t recognize what the relationship really is.
The examiners at the Lieber Foundation went basically further in finding the systems that make dopamine receptors a gamble factor.
The system exists explicitly in a subtype of the dopamine receptor, called the autoreceptor, which lies on the “male” side of the association between neurons, the presynaptic terminal. This autoreceptor manages how much dopamine is let out of the presynaptic neuron. Assuming autoreceptors are compromised, the progression of dopamine inside the mind is inadequately controlled, and a lot of dopamine streams for a really long time.
The agents found that diminished articulation of this autoreceptor in the mind makes sense of the hereditary proof of hazard for disease. This is steady with the common speculation that a lot of dopamine assumes a part in psychosis, and solid proof that the dopamine-schizophrenia enigma has finally been settled.
The spearheading neuroscientist Dr. Sol Snyder hailed the concentrate as a leading edge numerous a long time really taking shape. Dr. Snyder is a recognized help teacher of neuroscience, pharmacology and psychiatry and pioneer behind the Branch of Neuroscience at the Johns Hopkins College Institute of Medication, which bears his name. He was the researcher who found that antipsychotic drugs work by lessening mind dopamine.
“There’s heaps of jumbled information showing the pertinence of dopamine and dopamine receptors in schizophrenia,” said Dr. Snyder, who was not engaged with this examination project. “The key thing these scientists have done is to gather information that assembles everything and in a style that is powerful in laying out that dopamine frameworks are messed up in schizophrenia, and that is causal to the illness.”
“For quite a long time, individuals have discussed the dopamine association with schizophrenia,” Dr. Snyder said. “They used to say, ‘Indeed, this is intriguing to guess about, yet there’s no strong proof.’ Yet since we have considerably more thorough information accessible, we hold returning to a similar story. You don’t need to call it a theory any longer.”
More information: Jennifer Erwin et al, Analysis of the caudate nucleus transcriptome in individuals with schizophrenia highlights effects of antipsychotics and new risk genes, Nature Neuroscience (2022). DOI: 10.1038/s41593-022-01182-7
Journal information: Nature Neuroscience