Ovarian cancer remains the fifth leading cause of cancer-related deaths among women despite recent advancements, and new treatment options are urgently required, particularly for advanced cancers that recur after standard treatment. A preclinical study that was carried out under the direction of researchers from the Perelman School of Medicine at the University of Pennsylvania confirmed the existence of a brand-new target for drug-resistant ovarian cancer and provided data to support a treatment strategy that is currently being tested in clinical trials.
The findings (Abstract #1133) will be presented by Sarah Gitto, Ph.D., an instructor of pathology and laboratory medicine, at the 2023 Annual Meeting of the American Association for Cancer Research (AACR).
Senior author Fiona Simpkins, MD, a professor of Obstetrics and Gynecology, stated, “Unfortunately, the majority of ovarian cancers recur and become resistant to standard platinum chemotherapy.” Platinum-safe ovarian malignant growth is the most provocative sort of ovarian disease to treat, and growing new treatments in this space is a pressing need.”
“Unfortunately, most ovarian cancers recur and develop resistance to standard platinum chemotherapy.” Platinum-resistant ovarian cancer is the most difficult form to cure, and discovering novel medicines in this area is a top focus.”
Senior author Fiona Simpkins, MD, a professor of Obstetrics and Gynecology.
Newer targeted standard-of-care treatments called PARP inhibitors (PARPi) have improved ovarian cancer patients’ chances of survival; however, just like chemotherapy, these treatments eventually fail many patients, leaving them with no other options for treatment.
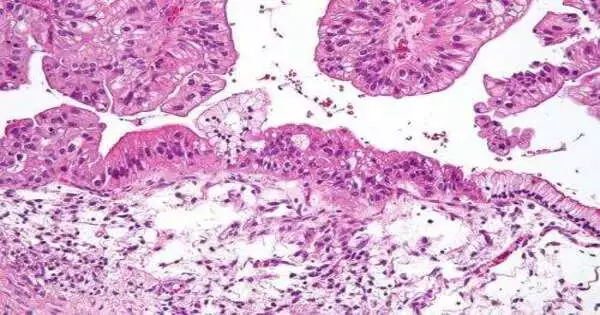
To battle these difficulties, this study zeroed in on the protein B7-H4, which — as urgent work from co-creator and teammate Daniel J. Powell Jr., Ph.D., an academic partner of Pathology and Research Center Medication has shown — is a possibly high effect protein that is tracked down in most bosom and ovarian diseases. The researchers wanted to find out if B7-H4 was still expressed at high levels after multiple treatments in the recurrent setting, making it an appropriate target for patients who have already received chemotherapy or PARPi. This is because cancer treatment can change which proteins are expressed on cells.
The group utilized matched examples from the Penn Ovarian Malignant Growth Exploration Center Cancer BioTrust
Assortment to check whether B7-H4 was found in growth tissue from similar patients previously, during, and after therapy—aand at times in the setting of end-stage metastatic sickness. They discovered that B7-H4 was overexpressed in 92% of high-grade serous ovarian carcinoma (HGSOC) tumors analyzed at diagnosis and remained elevated throughout cancer treatment, even after PARPi or chemotherapy. Critically, the protein was reliably tracked down outside the phones (as opposed to just inside the phones), where a medication could be attached without much of a stretch.
The researchers tested an antibody-drug conjugate in multiple cell lines and more than 20 patient-derived xenograft (PDX) cancer models of breast and ovarian cancer after establishing B7-H4 as a viable target. Neutralizer drug forms are another class of profoundly designated immunotherapy that is undeniably less harmful than conventional chemotherapy.
After just one dose, the tumors decreased in size in 61% of PDX models that had not previously been treated with chemotherapy or PARPi. With treatment proceeding like clockwork, to more readily copy clinical dosing, the medication brought about critical growth relapse and expanded endurance in treatment-safe PDX models.
Gitto stated, “We saw excellent anti-tumor activity, which is uncommon and sustained over a long period of time in models that are drug-resistant.” We have demonstrated that B7-H4 is an extremely robust and widespread target that can be utilized at various stages of patient care.”
A multisite Phase I clinical trial (NCT05123482) is currently testing a B7-H4-targeting antibody-drug conjugate.
“This work shows that antibody-drug conjugates merit further development in ovarian cancer,” Simpkins stated. “We’re excited about the potential for antibody-drug conjugates to overcome drug resistance.” Patients who participate in research, including biospecimen banking programs that enable scientists to learn about how their disease changes over time, make this kind of progress possible.
On Sunday, April 16, Gitto presented the findings at the Innovative Therapeutic Approaches Minisymposium.
More information: Abstract #1133