The body’s inflammatory cytokines, which react to allergens and cause excessive mucus production, wheezing, and difficulty breathing, have been the primary focus of allergy and asthma research and treatment for many years. Drugs that are frequently prescribed to patients, such as omalizumab, dupilumab, mepolizumab, and reslizumab, lower or block the various cytokines and antibodies that are responsible for the asthmatic response. However, their effects only take effect once a patient’s airway inflammation is well established.
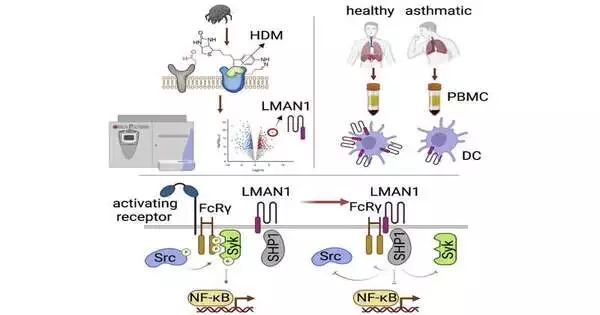
Dr. Tigno-Aranjuez sought a novel strategy for preventing allergen receptors from reacting in the first place. As a result, she used a method known as LRC-TriCEPS to identify cell receptors for a common allergen, the house dust mite. The technology demonstrated a cell protein known as LMAN1 that was previously unknown to play a role in the body’s response to allergens.
Cell Reports recently published her findings.
“We wanted to know, ‘What is this protein?’ when we first made this discovery. What is known so far about LMAN1’s function as an allergen receptor? She continued, “And the interesting thing was that people had not been paying much attention to this protein in the context of allergic asthma or allergy.”
“Our thinking is that this may not be limited to dust mites because many other allergens are mannosylated; this could be a very broad receptor that recognizes a wide range of allergens,”
Dr. Tigno-Aranjuez
LMAN1 was commonly referred to as a cargo receptor prior to her discovery—a protein that transports other proteins within and outside the cell. However, Dr. Tigno-Aranjuez demonstrated that LMAN1 and allergens from house dust mites can bind to the cell surface to trigger an allergic or inflammatory response. Her study also demonstrated that the house dust mite allergens’ specific mannose sugar structures were necessary for binding. Since many other common allergens, like pollen and fungi, are mannosylated—changed by adding mannose sugars—this discovery has a lot of potential.
“Because many other allergens are mannosylated, our thinking is that this may not be limited to dust mites.” She went on to explain that “this could be a very broad receptor that recognizes many different allergens.” Understanding how LMAN1 recognizes dust mites and the consequences of such recognition could be applied to many other settings, which is what we are currently attempting to explore if you are thinking about potential therapies.
The Cleveland Clinic collaborates on Dr. Tigno-Aranjuez’s research on LMAN1. This study has a co-investigator in Dr. Bin Zhang, an associate professor at the Lerner Research Institute. Dr. Zhang is regarded as an authority on LMAN1.
According to Dr. Zhang’s explanation, “LMAN 1 has been largely known as a protein that is involved in transporting proteins from the inside of cells to the outside of cells.” This is the first study to demonstrate a brand-new function for LMAN1, which is to act as a receptor to bring proteins like allergens inside cells from the outside. This may open up a new treatment route.”
This research represents a step toward assisting these patients, as there are hundreds of thousands of cases of allergic asthma worldwide and hundreds of thousands in the United States.
“Asthma is so common that people sometimes think, “We’ve got a lot of treatments; we’ve covered it.” The fact of the matter is that we could always benefit from additional options and treatments. Dr. Tigno-Aranjuez stated, “Many treatments are expensive, cannot be covered by insurance, and can only be prescribed if certain clinical criteria are met. Therefore, any new treatment we can offer that has the potential to be more widely used will always be an improvement.”
Currently, Dr. Tigno-Aranjuez and her team are conducting research to support their hypothesis that LMAN1 also recognizes pollen and other mannosylated allergens. If this is true, it could have a big impact on how many of the most common allergens are treated in the future.
Dr. Tigno-Aranjuez came to the United States from the Philippines to study at Case Western University in Cleveland for her graduate and postdoctoral training. She joined UCF in 2015 and studies immune signaling pathways in chronic inflammatory conditions like asthma and Crohn’s disease.
More information: Madelyn H. Miller et al, LMAN1 is a receptor for house dust mite allergens, Cell Reports (2023). DOI: 10.1016/j.celrep.2023.112208