Today at the International Liver Congress 2021, leading hepatology researchers announced significant new developments in hepatitis research. This includes new information on antivirals to treat Hepatitis B and D, as well as the use of infusion chemotherapy with P-1 inhibitors to treat liver cancer.
In animal models, a new immunological treatment against the hepatitis B and D viruses, both of which can cause liver cancer, shows promising results. The findings of the treatment, which is being developed by researchers at Sweden’s Karolinska Institutet, have been published in the journal Gut.
Chronic hepatitis B and D virus infections are major causes of severe liver damage and liver cancer. Although there is a vaccine for hepatitis B, over 250 million people currently have chronic infections. The available treatment rarely results in the complete disappearance of the infection, implying that the risk of liver damage remains. The current treatment for chronic hepatitis D infection only cures about a quarter of patients.
The study demonstrates that this is a viable route and encourages us to continue developing this treatment for human use. We are now optimizing the protein-based component to enable large-scale production to pharmaceutical standards, followed by final safety studies before applying for our first study with human subjects.
Matti Sällberg
That is why researchers at Karolinska Institutet are developing a new type of treatment that will hopefully provide a lasting treatment response against both viruses. The treatment consists of two components designed to affect the immune system in different ways. First, a DNA-based vaccine is administered that activates the production of neutralising antibodies and T-cells against both viruses. Then, repeated doses of a protein-based vaccine are given to reinforce the activation of the immune system.
Chronic hepatitis B (CHB) can lead to potentially fatal conditions such as cirrhosis and hepatocellular carcinoma (HCC). Cirrhosis develops in about 20% of chronically infected patients, causing hepatic insufficiency and portal hypertension. Furthermore, these patients are 100 times more likely than non-carriers to develop hepatocellular carcinoma. Hepatitis B excreted antigen (HBeAg) is an important marker for HCC because HBeAg-positive individuals are at a higher risk of developing HCC.
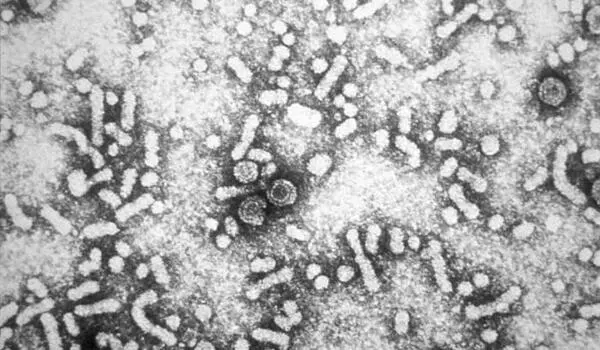
The newly published study shows that the treatment can protect cultured cells from HBV and HDV infection. When the treatment was given to mice carrying parts of the hepatitis B and D virus, which mimicked a chronic HBV infection, the animals produced high levels of the desired antibodies and T-cells.
Furthermore, antibodies from treated mice were able to protect mice carrying human liver cells from HBV and HDV infection at the same time. Furthermore, these antibodies were able to protect mice with chronic HBV infection from HDV infection. This is especially important because patients with chronic HBV infection are at risk of serious illness if infected with HDV.
“These are encouraging findings,” says Matti Sällberg, professor at Karolinska Institutet’s Department of Laboratory Medicine and one of the study’s two lead authors. “The study demonstrates that this is a viable route and encourages us to continue developing this treatment for human use. We are now optimizing the protein-based component to enable large-scale production to pharmaceutical standards, followed by final safety studies before applying for our first study with human subjects.”
The treatment was developed at the Department of Laboratory Medicine at Karolinska Institutet in Sweden. The tests in cell culture were done in collaboration with Heidelberg University in Germany and the experiments in mice carrying human liver cells were done in collaboration with Ghent University in Belgium.