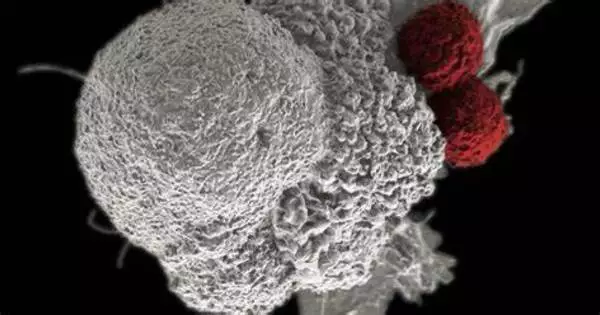
According to a new study from the University of Chicago, trans-vaccenic acid (TVA), a long-chain fatty acid found in meat and dairy products from grazing animals such as cows and sheep, improves the ability of CD8+ T cells to infiltrate tumors and kill cancer cells.
The study, published this week in Nature, also found that patients with higher levels of TVA in their blood responded better to immunotherapy, implying that it could be used as a nutritional supplement to supplement clinical cancer treatments.
“There are many studies attempting to decipher the link between diet and human health, and understanding the underlying mechanisms is extremely difficult due to the wide variety of foods people eat. However, if we focus solely on nutrients and metabolites derived from food, we can see how they influence physiology and pathology,” said Jing Chen, PhD, the Janet Davison Rowley Distinguished Service Professor of Medicine at UChicago and one of the study’s senior authors. “By focusing on nutrients that can activate T cell responses, we found one that actually enhances anti-tumor immunity by activating an important immune pathway.”
By focusing on nutrients that can activate T cell responses, we found one that actually enhances anti-tumor immunity by activating an important immune pathway.
Jing Chen
Finding nutrients that activate immune cells
Chen’s lab studies how metabolites, nutrients, and other molecules in the blood influence cancer development and response to cancer treatments. For the new study, two postdoctoral fellows, Hao Fan, PhD, and Siyuan Xia, PhD, both co-first authors, began with a database of around 700 known food metabolites and assembled a “blood nutrient” compound library of 235 bioactive molecules derived from nutrients. They looked for compounds in this new library that could influence anti-tumor immunity by activating CD8+ T cells, a type of immune cell that is essential for killing cancerous or virally infected cells.
After the scientists evaluated the top six candidates in both human and mouse cells, they saw that TVA performed the best. TVA is the most abundant trans fatty acid present in human milk, but the body cannot produce it on its own. Only about 20% of TVA is broken down into other byproducts, leaving 80% circulating in the blood. “That means there must be something else it does, so we started working on it more,” Chen said.
The researchers then conducted a series of experiments with cells and mouse models of diverse tumor types. Feeding mice a diet enriched with TVA significantly reduced the tumor growth potential of melanoma and colon cancer cells compared to mice fed a control diet. The TVA diet also enhanced the ability of CD8+ T cells to infiltrate tumors.

The team also performed a series of molecular and genetic analyses to understand how TVA was affecting the T cells. These included a new technique for monitoring transcription of single-stranded DNA called kethoxal-assisted single-stranded DNA sequencing, or KAS-seq, developed by Chuan He, Ph.D., the John T. Wilson Distinguished Service Professor of Chemistry at UChicago and another senior author of the study. These additional assays, done by both the Chen and He labs, showed that TVA inactivates a receptor on the cell surface called GPR43 which is usually activated by short-chain fatty acids often produced by gut microbiota. TVA overpowers these short-chain fatty acids and activates a cellular signaling process known as the CREB pathway, which is involved in a variety of functions including cellular growth, survival, and differentiation. The team also showed that mouse models where the GPR43 receptor was exclusively removed from CD8+ T cells also lacked their improved tumor-fighting ability.
Finally, the team also worked with Justin Kline, MD, Professor of Medicine at UChicago, to analyze blood samples taken from patients undergoing CAR-T cell immunotherapy treatment for lymphoma. They saw that patients with higher levels of TVA tended to respond to treatment better than those with lower levels. They also tested cell lines from leukemia by working with Wendy Stock, MD, the Anjuli Seth Nayak Professor of Medicine, and saw that TVA enhanced the ability of an immunotherapy drug to kill leukemia cells.
Focus on the nutrients, not the food
The study suggests that TVA could be used as a dietary supplement to aid in various T cell-based cancer treatments, though Chen emphasizes that the optimal amount of the nutrient itself, not the food source, must be determined. There is a growing body of evidence about the negative health effects of eating too much red meat and dairy, so this study shouldn’t be used to justify eating more cheeseburgers and pizza; rather, it suggests that nutrient supplements like TVA could be used to promote T cell activity. Chen believes that other nutrients may have the same effect.
“There is early data showing that other fatty acids from plants signal through a similar receptor, so we believe there is a high possibility that nutrients from plants can do the same thing by activating the CREB pathway as well,” he said.
The new study also emphasizes the promise of this “metabolomic” approach to understanding how the components of our diet affect our health. Chen and his colleagues hope to create a comprehensive library of nutrients circulating in the blood in order to better understand their effects on immunity and other biological processes such as aging.
“After millions of years of evolution, there are only a couple hundred metabolites derived from food that end up circulating in the blood, so that means they could have some importance in our biology,” says Chen. “To see that a single nutrient like TVA has a very targeted mechanism on a targeted immune cell type, with a very profound physiological response at the whole organism level — I find that really amazing and intriguing.”