It is possible that neuroscientists have identified a small molecule that can restore visual function after an optic nerve injury. This type of research is ongoing, and it is important to note that findings from laboratory studies may not necessarily translate to human clinical trials. Further research would be needed to determine the safety and efficacy of such a molecule as a treatment for optic nerve injuries in humans.
Traumatic injury to the central nervous system (CNSbrain)’s spinal cord, and optic nerve is the leading cause of disability and the second leading cause of death worldwide. CNS injuries frequently result in catastrophic loss of sensory, motor, and visual functions, which is the most difficult problem confronting clinicians and researchers. City University of Hong Kong (CityU) neuroscientists recently identified and demonstrated a small molecule that can effectively stimulate nerve regeneration and restore visual functions following optic nerve injury, providing great hope for patients suffering from optic nerve injury, such as glaucoma-related vision loss.
“There is currently no effective treatment available for traumatic injuries to the CNS, so there is an immediate need for potential drug to promote CNS repair and ultimately achieve full function recovery, such as visual function, in patients,” said Dr. Eddie Ma Chi-him, Associate Head and Associate Professor in the Department of Neuroscience and Director of the Laboratory Animal Research Unit at CityU, who led the research.
There is currently no effective treatment available for traumatic injuries to the CNS, so there is an immediate need for potential drug to promote CNS repair and ultimately achieve full function recovery, such as visual function, in patients.
Dr. Eddie Ma Chi-him
Enhancing mitochondrial dynamics and motility is key for successful axon regeneration
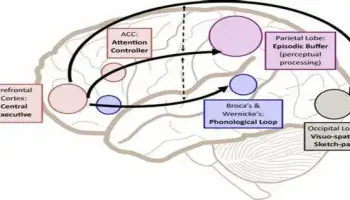
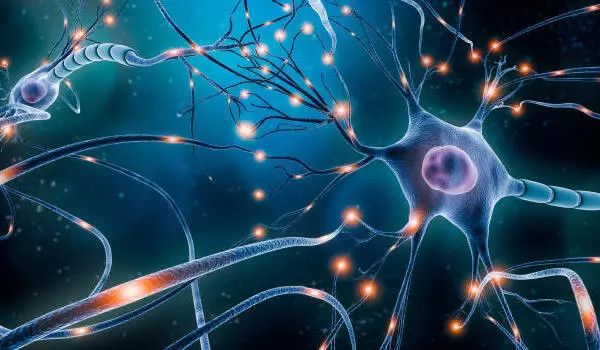
Axons are responsible for transmitting signals between neurons and from the brain to muscles and glands. They are a cable-like structure that extends from neurons (nerve cells). The formation of active growth cones and the activation of a regrowth program involving the synthesis and transport of materials to regrow axons is the first step toward successful axon regeneration. These are all energy-intensive processes that necessitate the active transport of mitochondria (the cell’s powerhouse) to injured axons at the distal end.
Injured neurons face unique challenges that necessitate long-distance transport of mitochondria from the soma (cell body) to distal regenerating axons, despite the fact that axonal mitochondria in adults are mostly stationary and local energy consumption is critical for axon regeneration.
Dr. Ma’s team discovered M1, a therapeutic small molecule that can increase mitochondrial fusion and motility, resulting in long-distance axon regeneration. In M1-treated mice, regenerated axons elicited neural activities in target brain regions and restored visual functions four to six weeks after optic nerve injury.
Small molecule M1 promotes mitochondrial dynamics and sustains long-distance axon regeneration
“Photoreceptors in the eyes [retina] forward visual information to neurons in the retina. To facilitate the recovery of visual function after injury, the axons of the neurons must regenerate through the optic nerve and relay nerve impulses to visual targets in the brain via the optic nerve for image processing and formation,” explained Dr. Ma.
The researchers assessed the extent of axon regeneration in M1-treated mice four weeks after injury to see if M1 could promote long-distance axon regeneration after CNS injuries. Surprisingly, the majority of regenerating axons in M1-treated mice reached 4mm distal to the crush site (near the optic chiasm), whereas no regenerating axons were found in vehicle-treated control mice. The survival of retinal ganglion cells (RGCs, neurons that transmit visual stimuli from the eye to the brain) in M1-treated mice increased significantly from 19% to 33% four weeks after optic nerve injury.
“This indicates that the M1 treatment sustains long-distance axon regeneration from the optic chiasm, i.e. midway between the eyes and target brain region, to multiple subcortical visual targets in the brain. Regenerated axons elicit neural activities in target brain regions and restore visual functions after M1 treatment,” Dr Ma added.
M1 treatment restores visual function
To further explore whether M1 treatment can restore visual function, the research team gave the M1-treated mice a pupillary light reflex test six weeks after the optic nerve injury. They found that the lesioned eyes of M1-treated mice restored the pupil constriction response upon blue light illumination to a level similar to that of non-lesioned eyes, suggesting that M1 treatment can restore the pupil constriction response after optic nerve injuries.
Furthermore, the researchers assessed the mice’s response to a looming stimulus — a visually induced innate defensive response to avoid predators. The mice were placed in an open chamber with a triangular prism-shaped shelter and a rapidly expanding overhead-black circle as a looming stimulus, and their freeze and escape responses were recorded. Half of the M1-treated mice responded to the stimulus by hiding in a shelter, demonstrating that M1 induced robust axon regeneration to reinnervate subcortical visual target brain regions for complete visual function recovery.
Potential clinical application of M1 for repairing nervous system injury
The seven-year study, which builds on the team’s previous research on peripheral nerve regeneration using gene therapy, highlights the potential of a readily available, non-viral therapy for CNS repair.
“This time, we used the small molecule M1 to repair the CNS simply by injecting it into the eyes, which is a well-established medical procedure for patients, such as macular degeneration treatment. Four to six weeks after the optic nerve was damaged, M1-treated mice showed successful restoration of visual functions such as pupillary light reflex and response to looming visual stimuli” Dr. Au Ngan-pan, Research Associate in the Department of Neuroscience, elaborated.
The team is also working on an animal model to treat glaucoma-related vision loss, as well as other common eye diseases and vision impairments like diabetes-related retinopathy, macular degeneration, and traumatic optic neuropathy. As a result, more research is needed to assess M1’s potential clinical application. “This research breakthrough heralds a new approach that could address unmet medical needs in accelerating functional recovery after CNS injuries within a limited therapeutic time window,” said Dr. Ma.