At the point when patients go through broad sedation, their mind’s movement frequently dials back as they sink into obviousness. Higher portions of sedative medications can prompt a considerably more profound condition of obviousness known as burst concealment, which is related to mental weaknesses after the patient awakens.
Brain wave signatures that could assist anesthesiologists in determining when patients are transitioning into that deeper state of unconsciousness have been discovered in a recent MIT study by analyzing the EEG patterns of patients undergoing anesthesia. This could empower them to keep patients from falling into that state, diminishing the risk of postoperative cerebrum brokenness.
The Proceedings of the National Academy of Sciences is where the work is published.
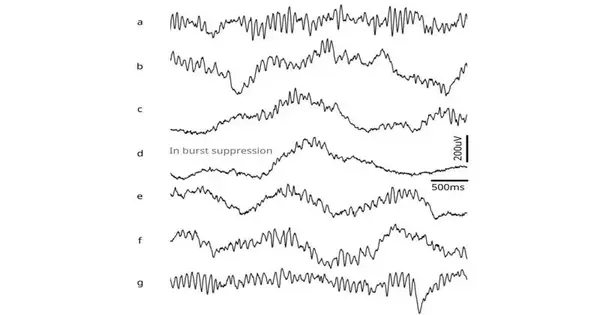
One of these unmistakable EEG designs arose in the cerebrum’s alpha waves (which have a recurrence of eight to 14 cycles per second). When patients became oblivious, these waves began to come and go in abundance. As patients went further into obviousness, the example of this fluctuating sufficiency, or adequacy tweak, consistently changed.
“If you track this modulation as it gets deeper or shallower, you have a very principled way to track the level of unconsciousness while under anesthesia,”
Emery Brown, the Edward Hood Taplin Professor of Medical Engineering and Computational Neuroscience.
“In the event that you track this regulation as it gets further or shallower, you have an exceptionally principled method for following the degree of obviousness under sedation,” says Emery Brown, the Edward Hood Taplin Teacher of Clinical Designing and Computational Neuroscience and an individual from MIT’s Picower Establishment for Learning and Memory and the Foundation for Clinical Designing and Science.
Brown is the senior creator of the new review. The lead creators of the paper are Picower Foundation research researcher Elie Adam, MIT graduate Ohyoon Kwon, and graduate understudy Karla Montejo.
Estimating mind waves
Mind waves, which are produced by synchronized neuronal action, sway at various frequencies depending on what sort of undertaking the cerebrum is performing. At the point when the cerebrum is firmly involved in mental movement, it produces higher-recurrence beta (15–30 hertz) and gamma (more noteworthy than 30 hertz) motions, which are accepted to assist with sorting out data and improve correspondence between various mind locales.
Normally utilized sedation medications, for example, propofol, fundamentally affect these movements. During sedation prompted by propofol or different sedatives that increment the viability of GABAergic inhibitory receptors in the cerebrum, the mind enters a condition of obviousness known as sluggish delta-alpha (SDA). This state is portrayed by sluggish (0.1–1 hertz), delta (1-4 hertz), and alpha (8–14 hertz) motions.
With higher dosages of these sedative medications, the cerebrum can fall into a considerably more profound state of obviousness. At the point when in this state, known as burst concealment, EEG accounts from the cerebrum show significant stretches of latency, accentuated by brief eruptions of low-plentifulness motions. At the point when patients enter this state, they are bound to encounter postoperative disarray, daze, and cognitive decline. Elderly patients are more likely to experience these effects, which can last for hours, days, weeks, or even months.
SDA and burst concealment produce unmistakable EEG designs that have been widely considered. Nonetheless, they have been concentrated as discrete mind states; what occurs during the progress between the two states is less clear. In this study, the MIT team set out to investigate that transition.
That’s what to do; the analysts concentrated on 10 solid workers and 30 patients who were going through a medical procedure. The majority of the patients got propofol intravenously, and the rest got sevoflurane, a commonly utilized sedative gas. Neuronal excitability is decreased by both of these medications because they target GABA receptors in the brain.
As the measurements of propofol were expanded, patients showed two particular examples of progress in their EEGs. The primary example was found in the alpha waves, which began to come and go. As the portion expanded, waxing was abbreviated and disappearing was delayed until the patient reached the condition of burst concealment.
“There is always a very strong modulation that you can see. As the adjustment becomes more significant, it in the end smooths out, and that is the point at which the cerebrum arrives at the more profound state,” Earthy colored says.
At the point when the amount of medication was decreased, the adequacy of the alpha waves started to increment once more.
The slow and delta waves in the patients’ EEG readings also showed a distinct pattern, according to the researchers. The slowest waves in the brain are called slow and delta oscillations. As the dose of the drug increased, the frequency of these waves got slower and slower, indicating that there was less activity in the brain.
Metabolic disturbance
The scientists speculate that Propofol has these impacts through its effect on neuron digestion. The medication is hypothesized to upset the development of ATP, the particles that cells use to store energy. As ATP creation declines, neurons become unfit to fire, prompting burst concealment.
“This is consistent with the perception that burst concealment is extremely continuous in more established patients, in light of the fact that their metabolic state might be less well managed than that of more youthful patients,” Earthy colored says.
The discoveries could offer anesthesiologists more refined command over a patient’s condition of obviousness during a medical procedure, says Brown. He currently desires to foster a calculation that could produce an admonition that a patient is moving toward burst concealment, which could be shown on a screen in the working room. He says that anesthesiologists could likewise figure out how to give that assurance by searching for these examples in a patient’s EEG.
“One reason we’re amped up for this is that it’s something you can really find in the crude EEG,” Earthy colored says. “Since we have called attention to these examples, they’re extremely simple to see.”
The scientists currently plan to additionally investigate what is befalling the cerebrum’s digestion during the progress to burst concealment, utilizing creature models.
More information: Adam, Elie et al, Modulatory dynamics mark the transition between anesthetic states of unconsciousness, Proceedings of the National Academy of Sciences (2023). DOI: 10.1073/pnas.2300058120