Each year, approximately 1 in 5 Americans withstand a traumatic brain injury brought on by a fall, car accident, or sports injury, which can result in both short- and long-term disability.
To better understand what transpires in the brain during injury, researchers from the University of Maryland School of Medicine (UMSOM) carried out a study in mice to examine how various types of brain cells in mice respond to severe trauma. In a recent study, which was published in the January issue of Autophagy, it was discovered that the internal recycling function of the immune system cells in the brain slowed noticeably after traumatic brain injury, allowing waste to accumulate and obstructing injury recovery.
The researchers also discovered that administering a drug to promote cellular recycling to mice with traumatic brain injury enhanced the mice’s capacity to recover from injury and complete a water maze, a test of their memory function.
“It’s possible that creating medications for people that encourage cellular recycling might reverse or prevent damage from traumatic brain injury, as we showed in our animal experiments. We are continuing to understand more about the molecular and cell biology pathways in trauma so that we may design treatments in a more directed manner.”
lead researcher Marta Lipinski, Ph.D., Associate Professor of Anesthesiology and Anatomy & Neurobiology at UMSOM.
According to lead researcher Marta Lipinski, Ph., “Many drugs and potential treatments have been proposed to treat traumatic brain injury, but none have ever worked in practice. D., a member of the Shock, Trauma, and Anesthesiology Research (STAR) Center at the University of Maryland Medical Center (UMMC) and Associate Professor of Anesthesiology, Anatomy, and Neurobiology at UMSOM. We observed damage from traumatic brain injury in our animal studies, so it’s possible that creating medications for patients that encourage this cellular recycling will help to reverse or prevent this damage. In order to use a more directed approach for creating solutions, we are constantly learning more about the molecular and cell biology mechanisms in trauma.”.
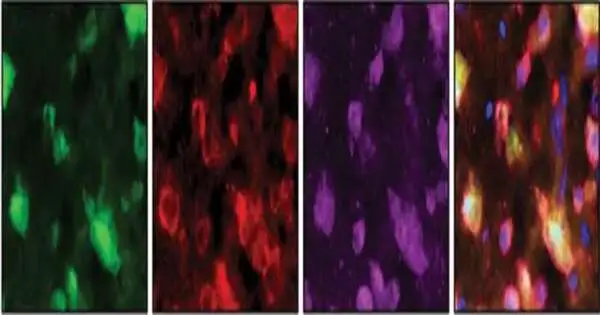
Autophagy is the process by which the body’s cells regularly recycle their own worn-out or damaged components that amass from regular wear and tear, infection, or injury. That method is used by the majority of brain cells to recycle smaller amounts of their own waste. In a prior study, Dr. Lipinski’s team demonstrated that traumatic brain injury decreased the capacity of neurons—the cells that transmit electrical impulses—to recycle their own damaged parts, which then resulted in the death of these neurons. The brain’s resident immune cells, known as microglia, can engulf, digest, and recycle entire damaged or dead cells in the tissue, but some brain cells are capable of even greater recycling feats.
White blood cells, which are typically kept out of the brain by the blood-brain barrier, can enter the brain after a traumatic brain injury and work with the microglia cells to eat and remove damaged cells. In this new study, Dr. Dorot Lipinski’s team examined the immune cells—microglia and white blood cells—in the brain following traumatic brain injury and discovered that, like the neurons, their recycling function was suppressed.
“Dr. It is crucial for neuroscientists to fully comprehend the complex system involved in a traumatic brain injury, according to Dean Mark Gladwin, MD, Vice President for Medical Affairs at the University of Maryland, Baltimore, and the John Z. Lipinski Professor of Neuroscience. also Akiko K., UMSOM’s Bowers Distinguished Professor. It is important to comprehend these cell-to-cell interactions and the effects that each cell type has on the ecosystem of the brain in order to create effective drugs for the treatment of traumatic brain injury.”.
Dr. Dorota Lipinski and her team blocked one of the crucial proteins required to carry out the immune cell’s recycling function in the brains of mice with traumatic brain injury in order to show the full impact of the recycling process on injury and recovery. The cell recycling processes in these mice were even more severely suppressed, which led to increased brain inflammation. They even performed worse than the mice, who only had brain damage when it came to being able to navigate the water maze. These findings suggested that recovery from brain injury depends on the immune cells’ ability to recycle themselves in the brain. Increasing it, on the other hand, might lessen the trauma’s effects.
Rapamycin, a medication typically used to treat cancer or prevent organ rejection, was used by the researchers to stimulate cellular recycling in the brains of mice who had suffered traumatic brain injuries in order to test that theory. Researchers discovered that after treatment, the mice’s brain inflammation levels decreased, and these mice performed better in the water maze.
Dr. Dorota Lipinski explained that the medication used in the study “blocks a set of proteins that are important for regenerating the body’s cells” and therefore cannot be used for prolonged periods of time. We need to carry out more research in this area to pinpoint the precise mechanism by which autophagy guards against neurological damage so that we can develop more specialized medications that boost this process without interfering with the crucial proteins required for the brain to regenerate.”.
More information: Nivedita Hegdekar et al, Inhibition of autophagy in microglia and macrophages exacerbates innate immune responses and worsens brain injury outcomes, Autophagy (2023). DOI: 10.1080/15548627.2023.2167689