The frequency of excess-related heart failures dramatically increased in Ruler Province, Washington, from 2015 to 2021, with the greatest increment among individuals who had consumed narcotics along with energizers, as per another review. That medication profile was likewise the most deadly among the four profiles assessed.
The discoveries are alarming on the grounds that crisis clinical reactions to sedate excesses are flooding networks across the US, the creators wrote. The paper was distributed today at the JAMA Organization Open.
“Chronic drug use and going too far are extending general wellbeing crises. Late reports recommend that the examples and kinds of medication use are changing, with many excesses including more than narcotics alone,” said the lead creator, Dr. Neal Chatterjee, a cardiologist and electrophysiologist at the UW Medication Heart Establishment in Seattle.
“Public health emergencies are growing as a result of drug addiction and overdose. According to recent research, drug usage patterns and varieties are evolving, with many overdoses incorporating substances other than opioids alone.”
Lead author, Dr. Neal Chatterjee, a cardiologist and electrophysiologist at the UW Medicine Heart Institute in Seattle.
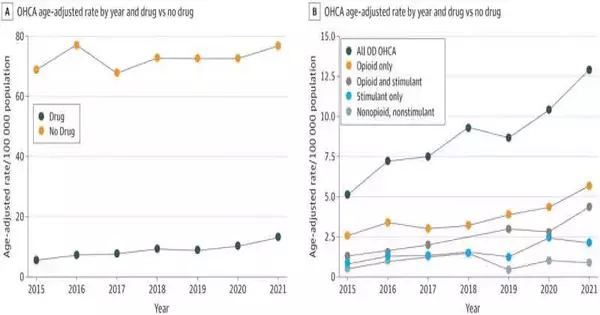
In clinical reports, generally out-of-medical clinic heart failures (OHCA) that include a medication glut are recorded essentially as “OD” without distinguishing explicit medications or medication types. In this review, the specialists looked at OD-related bodies of evidence against those not OD-related and furthermore worked with the clinical analyst to separate the medication-included cases into four subgroups: narcotic just, energizer just, narcotic joined with energizer, and other nonopioid, nonstimulant drugs.
Narcotics included fentanyl, heroin, hydromorphone, methadone, opium, codeine, and oxycodone. Energizers included amphetamines, methamphetamines, and cocaine.
The essential outcome measure for all gatherings was endurance to clinic release.
During the range (Jan. 1, 2015, to Dec. 31, 2021), Lord Area crisis clinical suppliers answered 6,790 calls in which somebody had encountered heart failure. Of those, 702 (10%) were not entirely set in stone to have involved a medication glut.
Chatterjee and partners found that Lord Area’s frequency of OD-involved OHCA had dramatically increased during the six-year range, with no related expansion in the occurrence of OHCA not including OD.
Toward the end of 2021, in spite of the fact that narcotics were just the medication profile most usually engaged with OHCA, the opioid-stimulant profile had developed to almost a similar occurrence, the paper revealed. Chatterjee said this finding lends itself to the drumbeat of reports describing narcotics, specifically fentanyl, as a vitally general wellbeing danger.
Additionally, the opioid-stimulant blend was associated with more awful endurance than narcotics alone or energizers alone. Chatterjee estimated that this may be because of the double organ effect of narcotics, which principally influence the respiratory framework, and energizers, which can expand the risk of heart arrhythmias.
“I think our review gives a significant setting while directing and really focusing on people who utilize unlawful medications,” he said. “For instance, ongoing subjective study information recommends that some of what might be driving an expansion in blended illegal medication use is the misperception that energizers can work on the wellbeing of, or improve the high connected with, depressants, for example, narcotics.
“Given our discoveries that blending these medications was related to the least endurance in heart failure cases, our review empowers the people who work in fixation medication to feature these risks.”
Chatterjee likewise said the review discoveries don’t propose that crisis responders’ profoundly coordinated revival conventions ought to change when a heart failure case is thought to be connected with drug glut.
“There isn’t right now a laid-out revival convention intended for OD-related OHCA,” he said. “Contemporary rules suggest specialists like naloxone (to invert narcotic excess) solely after a heartbeat is reestablished, but not as a component of the essential revival convention. By and large, this shows loads of opportunity to get better. Whether custom-made revival conventions for OD-OHCA could further develop results is an area of future review.”
More information: Vidhushei Yogeswaran et al, Presentation and Outcomes of Adults With Overdose-Related Out-of-Hospital Cardiac Arrest, JAMA Network Open (2023). DOI: 10.1001/jamanetworkopen.2023.41921 jamanetwork.com/journals/jaman … /fullarticle/2811464