According to animal and cell research, as retinal cells die in degenerative eye illnesses, they cause other cells to become hyperactive, causing noise that further obscures vision. Human tests to show this are, however, difficult to carry out. Antabuse, a licensed treatment used to wean individuals off alcohol, should dampen this hyperactivity and definitively establish whether hyperactivity has a role in humans, thereby fueling research into better drugs to help persons with progressive visual loss.
Researchers at the University of California, Berkeley, discovered that medicine once commonly used to wean alcoholics off alcohol improves vision in mice with retinal degeneration. The medicine has the potential to restore sight in people with the genetic disease retinitis pigmentosa (RP) as well as other vision problems such as age-related macular degeneration.
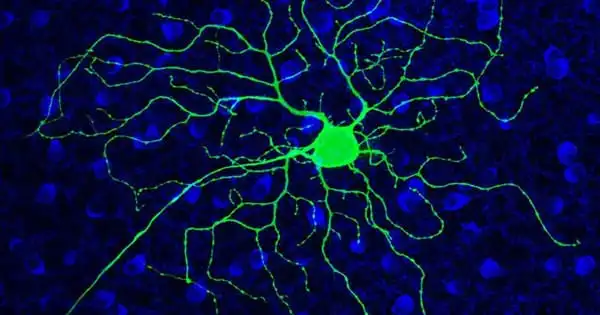
Previously, a group of scientists led by Richard Kramer, UC Berkeley professor of molecular and cell biology, demonstrated that retinoic acid is created when light-sensing cells in the retina called rods and cones die off gradually. This drug promotes hyperactivity in retinal ganglion cells, which normally relay visual information to the brain. The hyperactivity interferes with their encoding and transport of information, obstructing vision.
However, he discovered that the drug disulfiram, better known as Antabuse, inhibits not only enzymes involved in the body’s ability to digest alcohol, but also enzymes involved in the production of retinoic acid. Kramer and coauthor Michael Goard, who leads a lab at UC Santa Barbara (UCSB), showed that disulfiram therapy reduced retinoic acid synthesis and improved the detection of images displayed on a computer screen in nearly-blind mice.
Kramer believes that retinoic acid serves a similar impact in patients who have vision loss. However, because detecting retinoic acid in the eye would be excessively invasive, no human studies have been conducted.
There may be a long window of opportunity where suppressing retinoic acid with drugs like disulfiram could significantly improve low vision and make a real difference in people’s quality of life. Because the drug is already FDA-approved, the regulatory hurdles are low. It wouldn’t be a permanent cure, but right now there are no available treatments that even temporarily improve vision.
Richard Kramer
Disulfiram, which is already licensed by the Food and Drug Administration (FDA), may be able to demonstrate that link. The researchers intend to collaborate with ophthalmologists to undertake a clinical trial of disulfiram on RP patients. The trial would involve a small group of persons who have advanced but not yet total retinal degeneration.
“There may be a long window of opportunity where suppressing retinoic acid with drugs like disulfiram could significantly improve low vision and make a real difference in people’s quality of life,” said Kramer, the CH and Annie Li Chair in Molecular Biology of Diseases at UC Berkeley and a member of the Helen Wills Neuroscience Institute on campus. “Because the drug is already FDA-approved, the regulatory hurdles are low. It wouldn’t be a permanent cure, but right now there are no available treatments that even temporarily improve vision.”
Kramer, Goard and their colleagues — Michael Telias, a former UC Berkeley postdoctoral fellow now at the University of Rochester Medical Center, and Kevin Sit of UCSB — will publish their findings March 18 in the journal Science Advances.
Kramer acknowledged that disulfiram may not be for everyone. When combined with alcohol consumption, the drug can have severe side effects, including headache, nausea, muscle cramps and flushing.
“If you’re on the medicine and you take a drink, you’ll suffer the worst hangover of your life,” he claimed, “and that’s why it’s such a strong barrier to consuming alcohol.”
However, if disulfiram can enhance vision, more targeted medicines that do not interfere with alcohol breakdown or other metabolic activities may be investigated. The researchers have already tested an experimental medicine called BMS 493 that inhibits the retinoic acid receptor, as well as an RNA interference approach (a sort of gene therapy) to knock down the receptor. Both of these treatments significantly improved vision in RP mice.
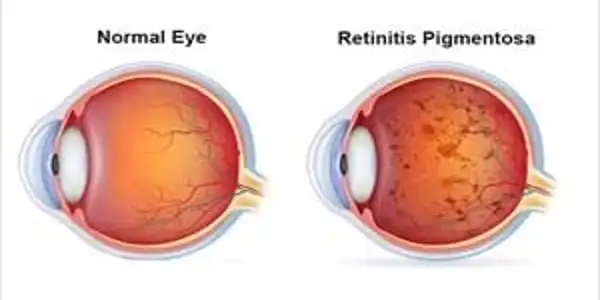
Photoreceptor breakdown
Three years ago, Kramer and his colleagues reported that retinoic acid generated sensory noise that interfered with remaining vision in mice with RP in the same way that ringing in the ears, known as tinnitus, can interfere with hearing in people who are losing vibration-sensitive cells in the inner ear. They showed that inhibiting the retinoic acid receptor reduced the noise and increased simple light avoidance behaviors in those mice.
But do mice treated with the drugs actually see better?
The latest study demonstrates that they do. First, the mice were trained to recognize and respond to a basic visual of black and white stripes flashed on a computer screen when they were young and had healthy retinas. The image was exhibited again a month later, when most of the rods and cones had decayed. The researchers discovered that mice given disulfiram or BMS 493 responded well even when the image was unclear. Mice given a placebo, on the other hand, did not respond even when the visual was crisp and clear.
In a second study, the researchers used a special microscope and a fluorescent protein indicator to light up and assess the responses of hundreds of cells in the brain to far more complex visual stimuli — a Hollywood movie clip that was replayed multiple times. Individual cells in the brains of vision-impaired mice with RP responded preferentially to specific frames in the movie, and their responses were more stronger and more consistent than those of mice treated with disulfiram or BMS 493.
The responses were so consistent, according to Kramer, that the researchers were able to determine which precise scene had prompted the cell’s response, but only in mice given with one of the medications.
Kramer and his colleagues described the mechanism behind hyperactivity caused by degeneration in 2019. They discovered that retinoic acid, which is well-known as a signal for embryonic growth and development, floods the retina when photoreceptors (the rods, which are sensitive to low light, and the cones, which are required for color vision) die. This is due to the fact that photoreceptors are densely packed with light-sensitive proteins called rhodopsin, which contain retinaldehyde. When retinaldehyde can no longer be absorbed by rods and cones, an enzyme called retinaldehyde dehydrogenase converts it to retinoic acid.
By attaching to retinoic acid receptors, retinoic acid activates retinal ganglion cells. These receptors cause ganglion cells to become hyperactive, resulting in a continual buzz of activity that drowns out the visual scene and inhibits the brain from distinguishing between signal and noise. Drug developers could try to avoid this by creating drugs that inhibit retinoic acid production by retinaldehyde dehydrogenase or compounds that interfere with the retinoic acid receptor.
“If a blind person was given disulfiram and their vision improved even slightly, that would be a fantastic result in and of itself. However, it would strongly suggest that the retinoic acid pathway is involved in vision loss “Kramer stated. “And that would be an important proof of concept that could drive new drug development and a whole new strategy for helping to improve vision.”