For the first time, scientists have shown that inherited genetic variables are linked to variations in the visual brain systems of infants later diagnosed with autism.
This study, which was published in the American Journal of Psychiatry, found that alterations in the size, white matter integrity, and functional connectivity of six-month-old’s visual processing systems are visible well before they show symptoms of autism as toddlers. Furthermore, the prevalence of visual system abnormalities in the brain is linked to the severity of autism symptoms in their older siblings.
This is the first study to show that infants with older siblings who have autism, and who later develop autism as toddlers, have specific biological differences in visual processing regions of the brain, and that these brain characteristics appear before autistic symptoms appear, according to Jessica Girault, PhD, assistant professor of psychiatry at the UNC School of Medicine. The severity of the autism symptoms in the older siblings is related to the occurrence of those visual processing abnormalities.
“We’re beginning to parse differences in infant brain development that might be related to genetic factors,” said Girault, who is also a member of the Carolina Institute of Developmental Disabilities (CIDD).
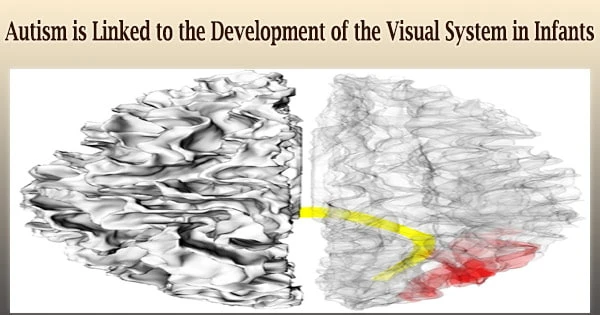
“Using magnetic resonance imaging (MRI), we studied selected structures of the brain, the functional relationship between key brain regions, and the microstructure of white matter connections between those brain regions. Findings from all three pointed us to the discovery of unique differences in the visual systems of infants who later developed autism.”
As part of the NIH-funded Infant Brain Imaging Study (IBIS) Network, UNC-Chapel Hill and Washington University researchers spearheaded this first-of-its-kind study.
Behind Baby’s Eyes
It’s not simply cute when parents and babies bond when they lock eyes and experience their world together day after day; it’s how kids learn to read small environmental cues. It’s the process by which babies learn to associate a caregiver’s actions with their own.
Using magnetic resonance imaging (MRI), we studied selected structures of the brain, the functional relationship between key brain regions, and the microstructure of white matter connections between those brain regions. Findings from all three pointed us to the discovery of unique differences in the visual systems of infants who later developed autism.
Girault
This visual rhythm is critical for cognitive, emotional, and social development during the earliest years of life. This discovery implies that something goes wrong in the brain’s visual system in babies who develop autism, affecting this visual interaction.
Researchers from the IBIS Network have recently employed MRI to document brain abnormalities in babies that acquire autism in their second year of life. Girault’s research published in 2020 found that if their elder autistic siblings had higher levels of autistic features, younger newborn siblings were much more likely to develop autism.
“This suggests that these autistic traits tell us something about the strength of genetic factors for autism within a family,” Girault said. “But we couldn’t say much more beyond that. This current study takes our work a step forward.”
The Infant Brain Imaging Study (IBIS) Network recruited 384 pairs of siblings for this study. Each pair’s older kid had already been diagnosed with autism, putting the infant sibling at a higher risk of developing the condition. The researchers then utilized several MRI techniques to examine the brains of the younger siblings at six, twelve, and twenty-four months of age.
The researchers evaluated brain volume, or the area of the brain surface, in the vision-related part of the brain (the occipital cortex), regions that had previously been shown to be altered in babies who went on to acquire autism as toddlers.
They also looked at the splenium’s white matter architecture, which had previously been linked to how rapidly babies orient to visual stimuli in their surroundings. Simultaneously, researchers recorded the extent of autistic features in the infants’ older autistic siblings.
The researchers discovered that brain elements related with the structure of the visual system varied in six-month-olds who went on to develop autism at 24 months of age compared to infants who did not acquire autism.
The researchers used this information to examine brain networks and discovered significantly poorer functional connections between specific brain networks associated to the visual system.
Girault and colleagues identified changes in the occipital gyrus, which is necessary for object recognition, and the splenium, which is important for communication between various hemisphere portions of the visual system. The splenium is also important for swiftly focusing our attention on what we observe.
“It is particularly notable that we were able to demonstrate associations between brain findings in infants and the behavior of their older siblings with autism,” said co-senior author John R. Pruett, Jr., MD, PhD, professor of psychiatry at the Washington University School of Medicine.
“The convergence of brain-wide, data-driven fcMRI results with the structural and diffusion findings strengthens our confidence in future replication of these discoveries, which could be tested in thenew cohort of 250 high-familial likelihood infants we are presently recruiting.”
Co-senior author Joe Piven, MD, CIDD director, added, “We think aberrant visual circuitry is a fundamental cog in the cascade of events leading to later autism. We think this circuitry alters how infants experience the world, and how they experience the world alters how their brains subsequently develop. It’s this secondary altered brain development that may result in what we call autism that typically emerges in the latter part of the first and second years of life.”
More research is needed, however this study suggests behavioral therapies focused at the visual and associated brain systems in newborns with a higher chance of developing autism due to hereditary risk factors in the first year of life. The goal of such interventions would be to reduce the chances of children getting particular, more severe autistic symptoms.
Co-senior authors are Joe Piven, MD, CIDD director, and Thomas E. Castelloe Distinguished Professor of Psychiatry and Pediatrics at the UNC School of Medicine; John Constantino, MD, the Blanche F. Ittleson Professor of Psychiatry and Pediatrics and at the Washington University School of Medicine and Psychiatrist-in-Chief at the St. Louis Children’s Hospital; and John R. Pruett, Jr., MD, PhD, professor of psychiatry at the Washington University School of Medicine.
This research was supported by grants from the National Institutes of Health (K01-MH122779, R01-HD055741, T32-HD040127, P30-HD003110, R01-MH118362, MH118362-02S1, and P30-NS098577), and by the Simons Foundation (140209).
All of the families and children that took part in the Infant Brain Imaging Study (IBIS) study are thanked by the authors. The IBIS Network is a cooperation of nine universities in the United States and Canada that is part of an NIH-funded Autism Center of Excellence project.