Interestingly, specialists have effectively utilized bacteriophages—infections that kill microbes—to treat an anti-infection safe mycobacterial lung contamination, making room for a young National Jewish Health patient with cystic fibrosis to get a day-to-day existence-saving lung relocation. The fruitful utilization of phages to treat Mycobacterium abscessus lung contamination was accounted for in a situation concentrate on distributed today in the diary cell.
“We had failed for a really long time to clear the mycobacterial contamination with an assortment of anti-infection agents,” said Jerry Nick, MD, lead author on the review and head of the Adult Cystic Fibrosis Program at National Jewish Health. “At the point when we utilized the microscopic organisms’ own regular adversaries, we had the option to clear the disease, which brought about a fruitful lung recolonization.”
“I am so appreciative of the work, ingenuity, and imagination of the relative multitude of individuals who were engaged with my treatment,” said Jarrod Johnson, beneficiary of the lung relocation. I thought I planned to kick the bucket. They have, in a real sense, saved my life. “
Cystic fibrosis is an acquired disease that causes the accumulation of thick bodily fluid in the lungs, resulting in rehashed bacterial contaminations that harm the lungs and can cause respiratory failure. new medicines have extraordinarily worked on the outlook for individuals with cystic fibrosis, the future actually remains essentially decreased.
“This study can serve as a blueprint for future use of phages to treat patients with severe Mycobacterium abscessus lung infection and save lives.”
Dr. Nick.
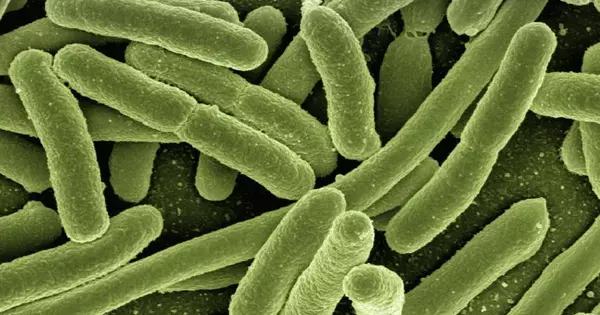
Mycobacteria are a typical and boundless family of microorganisms that can cause tuberculosis, sickness, and nontuberculous mycobacterial (NTM) contamination. Mycobacterium abscessus is an especially forceful and testing NTM contamination. Mixes of numerous anti-toxins and treatments lasting a year or longer are frequently ineffective. Public Jewish Health has the biggest grown-up cystic fibrosis program in the nation and is a main center for treatment of NTM contamination.
He is a 26-year-old cystic fibrosis patient who has experienced rehashed lung diseases all his life. As a kid, he was taken to different clinics a few times each year. As a grown-up, he encountered a fast decrease in his lung function following a diligent Mycobacterium abscessus contamination more than a six-year time span and got various ineffective medicines. By 2020, his lung work had fallen under 30%. Without a lung relocation, specialists felt he was probably going to pass on in a couple of years.
Johnson had been denied transfer by three transfer places, essentially due to his mycobacterial contamination. Mycobacteria can spread from the lungs to the skin and different tissues, which can torment relocating beneficiaries on immunosuppressive prescriptions. Dr. Scratch and his group at National Jewish Health thought about phages as a potential treatment choice. He was hospitalized at Saint Joseph Hospital in Denver, where he had spent over 200 days the prior year getting phage treatment.
Bacteriophages — or phages, for short — are infections that assault microbes. Interest in utilizing them to treat bacterial diseases has waned lately as an ever increasing number of microscopic organisms have become impervious to anti-microbials. Graham Hatfull, Ph.D., professor of Biological Sciences at the University of Pittsburgh and one of the review’s authors, is a pioneer in the discovery and use of phages to treat mycobacterial contaminations and provided the phages used to treat Johnson.
Phages are frequently explicit for a couple of types of microbes.In 2016, Dr. Scratch and his associates sent examples of the Mycobacterium abscessus from Johnson’s lungs looking for a phage that could kill the mycobacterium. Dr. Hatfull and his group in Pittsburgh screened many phage applicants and recognized two that proficiently killed the mycobacterium contaminating Johnson’s lungs. These were hereditarily designed to upgrade their true capacity.
“This examination can act as a guide for later utilization of phages to treat patients with extreme Mycobacterium abscessus lung disease and to save lives,” said Dr. Scratch.
Specialists at National Jewish Health got approval from the U.S. Food and Drug Administration for humane utilization of the trial treatment. Johnson accepted his most memorable imbuement of phages in September 2020, trailed by 500 days of two-day-to-day mixtures. In the span of two months, an assortment of genomic, cell culture, and clinical markers demonstrated that the treatment was succeeding. A little more than a year after the phage treatment started, Johnson’s disease seemed to have cleared.
Alice L. Dim, MD, Medical Director of the University of Colorado Lung Transplant Program, accepted the transfer was currently protected and put him on the dynamic rundown. He accepted his new lungs in October 2021 at the UCHealth Transplant Center, and as a team with Dr. Dim, stayed on phage treatment all through the system and during his recuperation. A scope of markers has demonstrated no proof of the disease following the transfer. Johnson has now stopped all treatment for Mycobacterium abscessus and is carrying on with an ordinary life.
Two other fruitful reactions of extreme Mycobacteria disease to phage have been accounted for by Dr. Hatfull’s group at the University of Pittsburgh. These cases were connected with patients, principally with skin contamination. The utilization of phages to treat a more extensive range of patients will assist in deciding the jobs of antibodies and phage opposition, directed by these fruitful contextual analyses.