Pancreatic cancer is a particularly deadly form of cancer, with a low survival rate in part because it is often not diagnosed until it has reached an advanced stage. However, recent research has shown promise in the development of biomarkers that can help identify individuals who are at an increased risk of developing pancreatic cancer, even before any symptoms have appeared.
A Duke Health research team has identified a set of biomarkers that could help determine whether pancreatic cysts are likely to develop into cancer or remain benign. The discovery, published online in the journal Science Advances, represents an important first step toward a clinical approach for classifying pancreatic lesions that are at high risk of becoming cancerous, potentially allowing their removal before they spread.
If successful, the biomarker-based approach could address the most significant barrier to lowering the risk of developing pancreatic cancer, which is on the rise and is notorious for growing silently before being discovered, often by chance, during abdominal scans.
“Even when pancreas cancer is detected at its earliest stage, it almost always has shed cells throughout the body, and the cancer returns,” said senior author Peter Allen, M.D., chief of the Division of Surgical Oncology at in the Department of Surgery at Duke University School of Medicine.
Our current focus is on locating it in cyst fluid. If we can find these distinct markers in cyst fluid, we may be able to perform a protein biopsy to determine whether we should remove the cyst before cancer develops and spreads.
Peter Allen
“That’s why we shifted our focus to these precancerous cysts, known as intraductal papillary mucinous neoplasms, or IPMNs,” Allen said. “Most IPMNs will never progress to pancreas cancer, but by distinguishing which ones will progress, we are creating an opportunity to prevent an incurable disease from developing.”
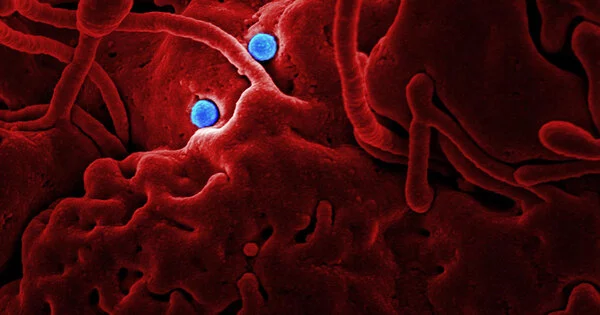
Allen and colleagues focused on specific areas of the cyst with high- and low-grade abnormal cell growth using a sophisticated molecular biology tool called digital spatial RNA profiling.
Previous methods for characterizing IPMNs were less precise and did not yield particularly accurate markers of cancer risk. However, digital spatial profiling allows researchers to analyze individual groups of cells. The Duke researchers were able to identify a number of genetic mutations that both fuel and potentially suppress pancreatic cancer development.
The researchers also discovered distinct markers for distinguishing between the two most common IPMN variants, as well as markers for defining a third common variant that results in less aggressive disease.
“We found very distinct markers for high-grade cell abnormalities, as well as slow-growing subtypes,” Allen said. “Our current focus is on locating it in cyst fluid.” If we can find these distinct markers in cyst fluid, we may be able to perform a protein biopsy to determine whether we should remove the cyst before cancer develops and spreads.”
Allen said current diagnostic strategies — including clinical, radiographic, laboratory, endoscopic, and cytologic analysis — have an overall accuracy of approximately 60%.
“Pancreatic cancer is on the rise, and if current trends continue, it will become the second-leading cause of cancer death in the United States in the next few years,” Allen said, adding that it’s unclear what’s causing cancer’s rise.
According to him, some studies suggest that inflammation plays a role. Allen is leading a clinical trial at Duke to see if anti-inflammatory therapy can reduce the development of cancer in IPMN patients.
While further research is needed to validate these findings and develop practical diagnostic tests based on these biomarkers, the early results are promising and could help improve early detection and treatment of pancreatic cancer.