Engineers have combined their transitory pacemaker into a coordinated network of four soft, flexible, wireless wearable sensors and control units positioned on several anatomically significant spots on the body. The sensors communicate with one another to continuously monitor the body’s numerous physiological activities, such as body temperature, oxygen levels, respiration, muscle tone, physical activity, and the electrical activity of the heart. The device then use algorithms to examine this combined activity in order to detect aberrant cardiac rhythms and determine when and at what rate to pace the heart.
Northwestern University researchers unveiled the world’s first transitory pacemaker, a completely implanted, wireless device that dissolves harmlessly in the body when no longer required. They have now unveiled a new, smarter version that is integrated into a network of four soft, flexible, wireless, wearable sensors and control units positioned around the upper torso.
The findings of the study will be published in the journal Science. Northwestern’s John A. Rogers, Igor R. Efimov, and Dr. Rishi Arora led the effort.
The sensors communicate with one another to continuously monitor the body’s numerous physiological activities, such as body temperature, oxygen levels, respiration, muscle tone, physical activity, and the electrical activity of the heart.
The device then use algorithms to examine this combined activity in order to detect aberrant cardiac rhythms and determine when and at what rate to pace the heart. All of this data is sent to a smartphone or tablet, allowing physicians to watch their patients remotely.
The good news is that this is only a transient condition. The heart regains its ability to stimulate itself after around five to seven days and no longer requires a pacemaker. The process for removing the pacemaker has substantially improved over the years, so problems are rare.
Igor R. Efimov
The new transient pacemaker and sensor/control network can be utilized in patients who require temporary pacing after cardiac surgery or who are waiting for a permanent pacemaker. The pacemaker wirelessly gathers energy from a network node – a small wireless device that softly clings to the patient’s chest. This method eliminates the need for external hardware, such as wires (or leads).
To allow the system to connect with the patient, the researchers included a small, wearable haptic-feedback device that may be worn anywhere on the body. When the sensors detect an issue (such as low battery power, incorrect device placement, or pacemaker dysfunction), the haptic device vibrates in specific patterns to notify wearers and educate them of the situation.
Insights from the experts
“This is the first time we have combined soft, wearable electronics with transitory electrical platforms,” added Rogers. “This approach has the potential to change the way patients receive care by providing multinodal, closed-loop control over essential physiological processes via a wireless network of sensors and stimulators that operates in a manner inspired by the complex, biological feedback loops that control behaviors in living organisms.”
“The technology untethers patients from monitoring and stimulation apparatuses that keep them restricted to a hospital setting for temporary cardiac pacing. Instead, patients might recover in the privacy of their own homes while benefiting from the peace of mind that comes with being electronically watched by their doctors. This would also lower health-care costs while freeing up hospital beds for other patients.”

“At the moment, temporary pacemakers require a cable that is attached to an external generator that stimulates the heart,” Efimov explained. “When the heart regains its ability to excite itself adequately, the wire must be removed. As you may expect, pulling a wire connecting to the heart is a rather dramatic surgery. We chose to address the subject from a new perspective. We developed a pacemaker that just dissolves and does not need to be removed. This avoids the risky process of taking out the wire.”
“Today’s pacemakers are highly clever and respond well to changing patient needs,” Arora explained. “However, the wearable modules perform all of the functions of traditional pacemakers and then some. The pacemaker is controlled by a patient wearing a little patch on their chest. The pacemaker is not only bioresorbable, but it is also controlled via a soft, wearable patch that allows the pacemaker to respond to normal living activities without the need for implantation sensors.”
Rogers is the Louis Simpson and Kimberly Querrey Professor of Materials Science and Engineering, Biomedical Engineering, and Neurological Surgery at Northwestern University’s McCormick School of Engineering and Feinberg School of Medicine, as well as the director of the Querrey Simpson Institute for Bioelectronics (QSIB). Efimov is a biomedical engineering professor at McCormick and a medicine (cardiology) professor at Feinberg. Arora is a Feinberg professor of medicine and the co-director of the Center for Arrhythmia Research.
‘Body-area network’
Rogers, a bioelectronics pioneer, has been working on soft, flexible, wireless wearable gadgets and bioresorbable electronic technology for for two decades. Rogers and his colleagues coupled and coordinated their bioresorbable, leadless pacemaker with four distinct skin-interfaced devices to function together in the new study. The skin-mounted devices are soft and flexible, and they can be gently peeled off after use, avoiding the need for surgical removal. After a time of use, the pacemaker degrades naturally in the body.
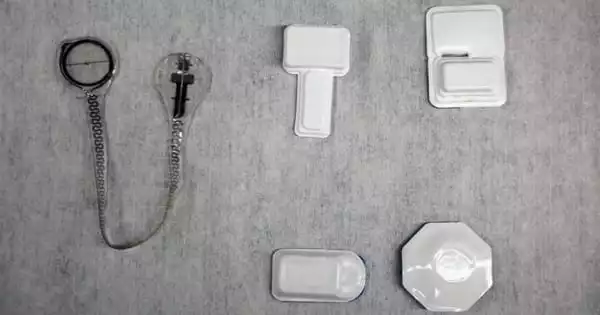
The “body-area network” includes:
- A temporary, bioresorbable, battery-free pacemaker to briefly pace the heart;
- A cardiac module that rests on the chest and provides power to and controls stimulation parameters for the pacemaker inserted as well as detects electrical activity and heart sounds.
- A hemodynamics module worn on the forehead that measures pulse oximetry, tissue oxygenation, and vascular tone.
- A respiratory module that sits at the base of the throat and monitors coughing and respiratory activity
- A multi-haptic-feedback module that vibrates and pulses in different patterns in order to interact with the patient.
“We wanted to show that it’s possible to deploy numerous distinct types of devices, each performing vital activities in a wirelessly coordinated manner across the body,” Rogers said. “Some people are detecting. Some are delivering power. Some are stimulating. Some are sending control signals. But they all work together, exchanging information, making decisions based on algorithms, and responding to changing conditions. The notion of several bioelectronic devices all communicating to one another and performing diverse activities at different important anatomical places is a frontier area that we will continue to study in the future.”
New advances, on-demand pacing
Since introducing Northwestern’s transitory pacemaker a year ago, the researchers have made numerous changes to advance the device. The prior device was flexible, but the new gadget is stretchy and flexible, allowing it to better suit the changing characteristics of a beating heart.
A biocompatible adhesive created in Rogers and Efimov’s labs is also used in the current generation. The adhesive enables the lightweight, thin device to softly laminate onto the surface of the heart without the use of sutures. Another significant advantage: while the temporary pacemaker degrades slowly and safely, it now releases an anti-inflammatory medication to prevent foreign-body reactions.
The device’s ability to offer pacing on-demand, based on when the patient requires it, is perhaps the most significant advancement. The chest-mounted cardiac module, which is linked to the pacemaker, records an electrocardiogram in real time to monitor heart function. The wireless technology was found to be as accurate and precise as clinical-grade systems when researchers compared it to gold-standard electrocardiograms in the study.
“The cardiac module basically orders the pacemaker to apply stimulus to the heart,” explained Efimov. “Pacing stops when regular activity is restored. This is significant because stimulating the heart when it is not essential increases the risk of arrhythmia.”
“The pacing system is completely autonomous,” said Yeon Sik Choi, a postdoctoral fellow in Rogers’ lab and co-first author of the paper. “It can automatically detect a problem and apply treatment. It’s easy and self-contained with minimal external needs.”
Health care gentle enough for newborns
Rogers, Efimov, Arora, and their teams believe their system will benefit the most vulnerable patients the most. Around 40,000 newborns are born each year with a hole in the wall that separates their heart’s upper chambers. Approximately 10,000 of these instances are life-threatening and require emergency surgery. Following surgery, all newborns are fitted with a temporary pacemaker.
“The good news is that this is only a transient condition,” Efimov explained. “The heart regains its ability to stimulate itself after around five to seven days and no longer requires a pacemaker. The process for removing the pacemaker has substantially improved over the years, so problems are rare. But we could free these babies from the wires connecting to an external generator and free them from needing a second procedure.”