Profound mind feeling (DBS) to the superolateral part of the average forebrain pack (MFB), which is connected to reward and inspiration, uncovered metabolic cerebrum changes north of a year post-DBS implantation, making it a solid likely treatment for treatment-safe gloom, as per scientists at UTHealth Houston.
The results of the review, which included 10 patients, were published today in Molecular Psychiatry.
“This is something that individuals have been attempting to accomplish for quite a while, yet we have not always been fruitful with involving DBS for mental diseases,” said first creator Christopher Conner, MD, Ph.D., a previous neurosurgery resident in the Vivian L. Smith Department of Neurosurgery at McGovern Medical School at UTHealth Houston. Yet, this PET review shows that we’re modifying the way in which the mind is working over the long haul and we are beginning to impact the manner in which the cerebrum begins to sort out itself and begins to handle data and information.” Conner is currently an individual with the University of Toronto.
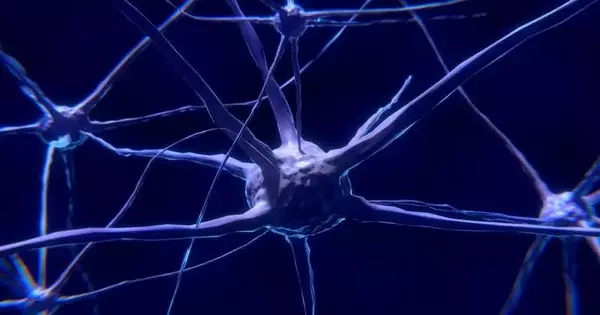
For quite a while, DBS has been utilized to treat patients experiencing developmental issues like Parkinson’s illness, quake, and dystonia, and has been concentrated on as a potential treatment for patients with treatment-safe gloom. In DBS, anodes are embedded into specific mind regions, where they create electrical motivations to influence cerebrum action.
“However, this PET study demonstrates that we are affecting how the brain functions over time, and we are beginning to change the way the brain organizes itself and processes information and data.”
Christopher Conner, MD, Ph.D., a former neurosurgery resident in the Vivian L. Smith Department of Neurosurgery
Nonetheless, finding which piece of the mind should be focused on to treat gloom over the long haul has been testing.
“We designated a heap of strands that pass through this little region in the brainstem to go to different regions all through the mind,” Conner said. “The PET sweeps showed that this little objective region makes diffuse downstream impacts. It’s not one single impact since there’s not one single region of the mind connected to gloom. The entire mind should be changed and through this one little objective, that is the thing we had the option to do. “
Scientists played out an underlying PET sweep before the DBS system on the 10 patients in the review for a gauge picture. They carried out extra PET sweeps at six and a year to survey changes after treatment. Sweeps of 8 of the 10 patients showed a reaction.
“A responder to the treatment implies that your downturn possibly diminishes by no less than half; you’re feeling improved,” said co-creator Joo de Quevedo, MD, Ph.D., teacher in the Louis A. Faillace, MD, Department of Psychiatry and Behavioral Sciences at McGovern Medical School.
“Thus, for patients with extreme ongoing treatment-safe gloom, diminishing our side effects by half is a ton. It’s the contrast between being impaired and having the option to follow through with something. Relating to the PET picture changes, our patients revealed that their downturn was reduced after the treatment. De Quevedo likewise fills in as head of the Translational Psychiatry Program and the Treatment-Resistant Depression Program, part of the Center of Excellence on Mood Disorders.
More information: Christopher R. Conner et al, Brain metabolic changes and clinical response to superolateral medial forebrain bundle deep brain stimulation for treatment-resistant depression, Molecular Psychiatry (2022). DOI: 10.1038/s41380-022-01726-0
Journal information: Molecular Psychiatry