Diet alters a gut microbe molecule, prompting immune cells to downregulate inflammation, according to mouse research. The study elucidates the molecular mechanism underlying the long-held belief that diet, microbiota, and immunity all influence one another in a variety of ways. If confirmed in larger animals and humans, the findings could help shape the development of small-molecule drugs that modulate immune responses to treat inflammatory conditions.
For hundreds of years, the adage “you are what you eat” has been used to illustrate the relationship between diet and health. An international team of researchers has now discovered molecular proof of this concept, demonstrating how diet ultimately influences immunity via the gut microbiome.
The study in mice reveals that what animals eat causes the release of a metabolic byproduct from a specific gut microbe, which modulates the animals’ gut immunity. The findings, which were published in Nature, provide a unifying explanation for the complex interplay of diet, gut microbiota, and immune function. Scientists from Harvard Medical School, Brigham and Women’s Hospital, Seoul National University, and Monash University in Australia collaborated to create them.
The experiments identify a microbial molecule the host diet influences whose synthesis and release. That molecule, in turn, activates and signals a subset of cells known as natural killer (NK) T cells, which are involved in immune regulation and have been linked to a variety of inflammatory conditions.
We have demonstrated how diet affects the immune system via a microbial mediator in the gut, and this is a really striking example of the diet-microbiota-immunity triad at work. What this work really does is provide a step-by-step pathway from start to finish that explains how and why this triad works and how diet ultimately affects the immune system.
Professor Dennis Kasper
While scientists have long suspected that diet affects immune health, the new study elucidates the precise molecular cascade behind this interaction, according to study senior author Dennis Kasper, professor of immunology at Harvard Medical School.
“We have demonstrated how diet affects the immune system via a microbial mediator in the gut, and this is a really striking example of the diet-microbiota-immunity triad at work,” Kasper said. “What this work really does is provide a step-by-step pathway from start to finish that explains how and why this triad works and how diet ultimately affects the immune system.”
If confirmed in larger animals and, eventually, in humans, the findings could aid in the development of small-molecule treatments that boost both intestinal and overall immunity, according to the researchers.
“Microbes in the gut produce molecules with a wide range of structural diversity. We used microbial and chemical tools to figure out how these molecules are made by gut bacteria and how they behave in the host gut” Sungwhan Oh, a principal investigator at Brigham and Women’s Hospital’s Center for Experimental Therapeutics and Reperfusion Injury and a former postdoctoral fellow in the Kasper lab, was the study’s first author. “Our findings provide fascinating insights into the microbiome, diet, and immune function, as well as intriguing clues about how molecules produced by our inner neighbors, can be used to design therapies.”
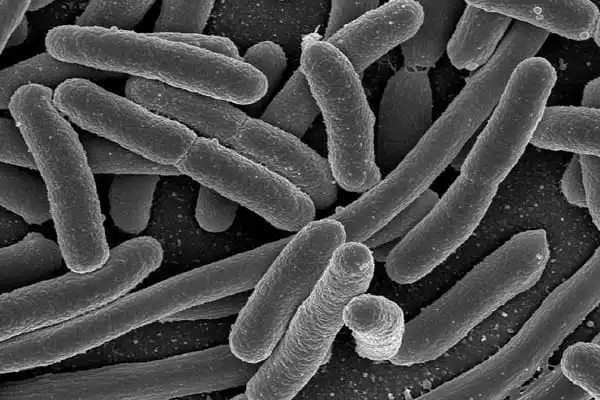
The team identified the immune-signaling cascade triggered by the metabolic breakdown of dietary amino acids in the mouse gut through a series of experiments. This multistep pathway begins with an animal consuming food containing branched-chain amino acids, so named because one of their molecular chains has a tree branch-like structure. The branched-chain amino acids are then taken up by B. fragilis, a gut-resident microbe, and converted into sugar-lipid molecules with branched chains by a specific enzyme. B. fragilis then releases branched-chain molecules that are spotted and picked up by antigen-presenting cells, which in turn induce NK T cells to exercise their immunoregulatory response by upregulating inflammation-controlling genes and immune-regulatory chemicals.
Notably, the experiments demonstrated that the cascade is initiated by the branching of the chain structure. Straight-chain molecule versions did not have the same effect. Furthermore, the researchers discovered that B. fragilis changes the structure of the sugar-lipid molecules it metabolizes, making them more capable of binding to receptors on specific immune cells and initiating a signaling cascade that results in inflammation reduction.
The research also revealed that three different branched-chain amino acids consumed by mice resulted in slightly different structural changes to the bacterial lipid molecules, resulting in different patterns of binding with immune cells.
Seung Bum Park, a chemistry professor at Seoul National University, synthesized and tested 23 different configurations of the microbe-made immunomodulatory molecule to determine how each one interacts with immune cells that regulate inflammation.
Experiments conducted by the Harvard team revealed that synthetic, lab-made branched-chain lipid molecules induced NK T cells to release the immune-signaling chemical IL-2, whereas straight-chained versions of these molecules did not. As a result of being activated, the NK T cells induced the expression of genes that regulate immunity but not genes that drive inflammation.
Jamie Rossjohn, professor of biochemistry and molecular biology at Monash Biomedicine Discovery Institute in Australia, used structural biology to determine how the lipid structure interacts with and binds to antigen presenting cells – the immune cells that give NK T cells the green light to produce anti-inflammatory chemicals.
Finally, the researchers gave the branched-chain sugar-lipid molecule to mice with ulcerative colitis. Animals treated with the branched-chain molecule fared significantly better than untreated animals. They not only gained weight, but when researchers examined the gut cells of the mice under a microscope, they discovered that there were no signs of colon inflammation in these cells.
The findings provide a structural and molecular explanation for the previously observed anti-inflammatory effects of this class of sugar-lipids produced by the gut microbe B. fragilis. “This work is an excellent example of transdisciplinary discovery-based research aimed at answering a major question in biomedical sciences, namely, how the interplay between diet and microbiota can modulate the immune system,” Rossjohn said.
Kasper and colleagues published a study in 2014 showing that a sugar-lipid molecule released by B. fragilis had anti-inflammatory effects on the gut and protected mice from colitis, but the scientists didn’t know how the microbe made these molecules or the specific structural features of the sugar-lipids that conferred the anti-inflammatory effect. The current study provides an answer to this question by demonstrating that the sugar-lipid molecules produced by this organism are branched-chain, and it is precisely this branched-chain structure that allows them to bind to immune cells and dampen their proinflammatory signaling.
“Our new work shows that the branching of the lipid structure induces a very different response the branching in the structure induces an anti-inflammatory rather than a proinflammatory response,” Kasper explained. According to the researchers, the findings give hope that inflammatory diseases mediated by these NK T cells could one day be treated with inflammation-dampening microbial molecules created in the lab.
The precise function of NK T cells the immune cells that the microbe-made molecule eventually activates to control colonic inflammation in mice – is unknown, according to Kasper. Given that these cells line the human gastrointestinal tract and lungs, as well as being found in the liver and spleen, they are likely to play an important role in immune regulation. Previous research suggests that these cells may play a role in a variety of inflammatory conditions, including ulcerative colitis, as well as in airway inflammatory conditions like asthma.
“We can never isolate enough of these immune-modulatory molecules from bacteria for therapeutic use,” Kasper explained, “but the beauty of this is that we can now synthesize them in the lab. The idea is to have a drug that can modulate inflammation in the colon and elsewhere.”