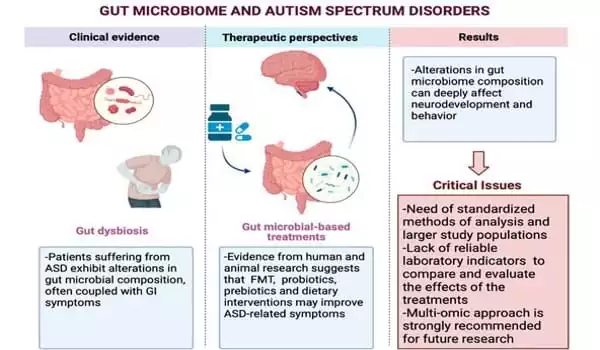
Diet influences host health by influencing the composition of the gut microbiota. It has been discovered that normal gut microbiota influences immune system development, nutrient absorption, tissue generation, morphogenesis, and bone homeostasis-metabolism. According to research, children with ASD often have a different mix of gut microbes than children who do not have the condition. In addition, when normal species of gut bacteria are absent in lab animals, autism-like symptoms appear.
Autism spectrum disorder (ASD) may be caused in part by differences in the composition of the gut microbiota, according to research, based on the observation that certain types of microbes are more common in people with autism. However, according to a paper published on November 11 in the journal Cell, the link may actually work the other way around: the diversity of species found in the guts of children with autism may be due to the restricted dietary preferences associated with autism, rather than the cause of their symptoms.
“There’s a lot of interest in the role of the gut microbiome in autism, but not a lot of hard evidence,” says senior author Jacob Gratten of Mater Research in Brisbane, Australia, in collaboration with The University of Queensland. “Our study, which is the largest to date, was designed to address some of the limitations of previous research.”
There’s a lot of interest in the role of the gut microbiome in autism, but not a lot of hard evidence. Our study, which is the largest to date, was designed to address some of the limitations of previous research.
Dr. Jacob Gratten
Over the last decade, as next-generation sequencing of microbial species in the gut has made microbiome analysis more automated and time-consuming, a number of studies have looked into the relationship between specific species of microbes in the gut and mental health. Not only has the gut-brain axis been linked to ASD, but also to anxiety, depression, and schizophrenia. The possibility of targeting the microbiota for new treatments is a growing area of research.
In the Cell study, researchers examined stool samples from 247 children ranging in age from 2 to 17. The samples were taken from 99 children with ASD, 51 undiagnosed paired siblings, and 97 unrelated, undiagnosed children. The participants in the study came from the Australian Autism Biobank and the Queensland Twin Adolescent Brain Project.
The samples were analyzed using metagenomic sequencing, which examines the entire genome of microbial species rather than short genetic barcodes (as with 16S analysis). It also provides gene-level information rather than just species-level information, and it provides a more accurate representation of microbiome composition than 16S analysis, which was used in many of the previous studies linking the microbiome to autism.
“We also carefully accounted for diet, as well as age and gender, in all of our analyses,” says first author Chloe Yap, an MD-PhD student who works with Gratten. “Because the microbiome is strongly influenced by the environment, we designed our study with two comparison groups.”
According to their findings, there is limited evidence for a direct link between autism and the microbiome. They did, however, discover a highly significant link between autism and diet, and that an autism diagnosis was associated with a less diverse diet and poorer dietary quality. Furthermore, psychometric measures of autistic traits (such as restricted interests, social communication difficulties, and sensory sensitivity) and polygenic scores (a genetic proxy) for ASD and impulsive/compulsive/repetitive behaviors were linked to a less diverse diet.
“When the data are analyzed together, they support a strikingly simple and intuitive model in which autism-related traits promote restricted dietary preferences,” Yap says. “As a result, there is less microbiome diversity and more diarrhea-like stool.”
The researchers acknowledge that the current work has several limitations. One limitation is that the study’s design does not rule out microbiome contributions prior to ASD diagnosis, nor does it rule out the possibility that diet-related changes in the microbiome have a feedback effect on behavior. Another limitation is that they could only account for the potential impact of antibiotics on the microbiome by excluding those who were taking these medications at the time of stool collection. Finally, there are currently no comparable datasets available to confirm the findings.
“We hope that our findings inspire others in the autism research community to routinely collect metadata in “omics” studies to account for important (but often overlooked) potential confounders like diet,” Gratten says. “Our findings also highlight the importance of nutrition for children with autism, which is a clinically important (but underappreciated) contributor to overall health and well-being.”
To replicate their findings, the researchers intend to collect new data from a larger sample.