Neutrophils, the most plentiful sort of white platelet, are the body’s most memorable line of defense against disease. Unfamiliar microbes can pressure the body and enact neutrophils. When enacted, neutrophils utilize different weapons to safeguard the body. Yet, in the event that they are overactivated, these weapons can harm the body’s own tissues. Lung tissue is soaked with veins, making them truly helpless to neutrophil assaults. Assuming adequate extreme, intense lung wounds can prompt intense respiratory pain disorder (ARDS), the main source of death because of coronavirus.
Nicholas Tonks, Caryl Boies teacher of disease research at Cold Spring Harbor Lab (CSHL), and his group have found a medication competitor that can forestall deadly lung irritation in mice by hindering a protein called PTP1B. Their revelation might assist in developing better medicines for extreme fiery circumstances like sepsis and coronavirus.
“At the point when you ponder the coronavirus, intense lung injury and ARDS underlie the lethal parts of the illness,” Tonks says. “As the pandemic took hold, we were considering whether there was anything we could do to help, to provide a better understanding of this part of the illness and propose ways it very well may be dealt with.”
“When it comes to COVID-19, acute lung injury and ARDS are at the heart of the disease’s fatality. So, when the pandemic hit, we wondered whether there was anything we could do to help, to provide an awareness of this part of the disease and to provide treatment options.”
Nicholas Tonks, Caryl Boies professor of cancer research at Cold Spring Harbor Laboratory (CSHL)
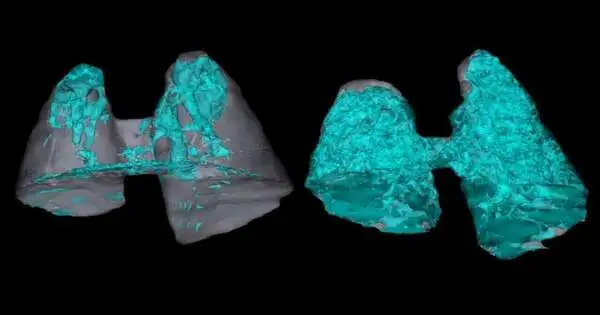
Tonks’ alumni understudy Dongyan Tune explored whether utilizing a PTP1B inhibitor drug competitor could hose the deadly results of overactive neutrophils in mice. She found that pretreating mice with the PTP1B inhibitor decreased lung tissue harm. When untreated, not exactly 50% of the mice endure intense lung wounds and ARDS. Yet, when pretreated, they generally make due.
The scientists took advantage of a characteristic cycle, called neutrophil maturation, that the body uses to control the safe cell’s life expectancy. As they age, neutrophils become less risky. Tonks’ group found PTP1B restraint speeds up neutrophil maturation. Tune explains it this way: “A matured neutrophil resembles an officer without a weapon.””So, paying little heed to the number of neutrophils that flood a region, they won’t have the option to cause serious harm.”
This task was important for a program of coronavirus related research at CSHL. Tonks expresses that joint efforts with CSHL teacher Mikala Egeblad, postdoc Jose M. Adrover, and CSHL Exploration Academic partner Scott Lyons were vital for this disclosure. Proceeding, he and Tune are attempting to build a comprehension of what PTP1B inhibitors mean for the safe framework. Tonks trusts his lab’s progress with research to prompt new medicines and safeguard measures for different fiery illnesses. His lab is presently working with DepYmed, Inc. to take PTP1B inhibitor drug applicants into clinical preliminaries.
Tonks’ lab concentrates on signal transduction, the cycle that controls how cells respond to signals from their current circumstances. Specifically, they center around the PTP protein family, which Tonks found a while back. From that point forward, he’s tried to foster little atom drug applicants that focus on these proteins, which can give new ways to deal with treating significant human illnesses, including malignant growth and metabolic and neurodegenerative sicknesses.
More information: Dongyan Song et al, PTP1B inhibitors protect against acute lung injury and regulate CXCR4 signaling in neutrophils, JCI Insight (2022). DOI: 10.1172/jci.insight.158199
Journal information: JCI Insight