Antibiotic use is fairly prevalent among breastfeeding moms, and there is a risk of transmission to infants via breast milk. While most drugs used by nursing moms do not harm their newborns, there are situations when they can have catastrophic implications.
Breast milk is without a doubt the finest type of nutrition for newborns and young infants. Its benefits extend far beyond nutritional and anti-infective properties. As a result, there are essentially no contraindications to breastfeeding, especially in underdeveloped nations where social, cultural, and economic factors frequently take precedence over medical concerns.
Infants carry a vast assemblage of bacteria, viruses and fungi in their guts. Combined, these microbes make up a complex ecology known as the gut microbiome, which plays a major role in health and disease throughout life. The initial source of these billions of microbes is the mother’s breast milk. Scientists have now used next-generation sequencing to investigate the breast milk microbiome from HIV positive women in Kenya.
Infants carry a vast assemblage of bacteria, viruses and fungi in their guts. Combined, these microbes make up a complex ecology known as the gut microbiome, which plays a major role in health and disease throughout life.
Efrem Lim and colleagues employ next-generation sequencing to analyze the breast milk microbiota of HIV positive women in Kenya in a new study. Lim is an assistant professor in Arizona State University’s School of Life Sciences and a researcher with the Biodesign Center for Fundamental and Applied Microbiomics. Breast milk samples from mothers who got antibiotic treatment were compared to those who received combined anti-retroviral therapy in the study. The findings reveal that antiretroviral medication alone has no effect on normal breast milk microbiome richness, variety, or bacterial composition, however antibiotics generate dramatic alterations in the microbiome.
The research appears in the current issue of the journal Microbiology Spectrum.
Currently, in many countries, even maternal HIV infection is not an absolute contraindication to breast feeding due to a lack of a safer and more cost-effective method of giving food. Although the majority of medicines given to breast-feeding women are safe for babies and there are few contraindications to breast-feeding when maternal medication is required, initiating and continuing breast-feeding by a mother on antibiotics remains a tough problem. On the one hand, the hazards have frequently been exaggerated, resulting in the avoidance of a necessary medicine or the discontinuation of breast feeding.
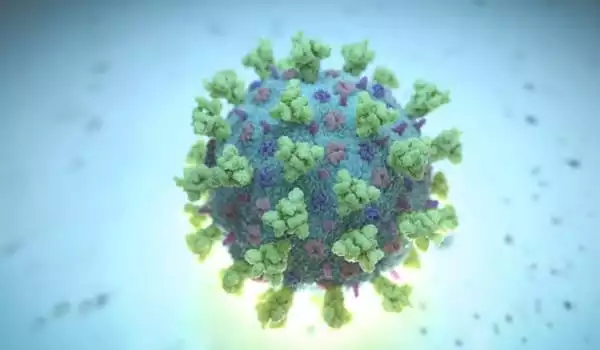
Breast milk delivers a healthy blend of vital bacteria, antibodies, and human milk oligosaccharides to developing infants (a form of carbohydrate). Breast milk is used by nursing newborns to create the suite of bacteria that begin to develop in their stomach immediately after birth. Microbes found in infant stool samples can be traced back to the mother’s breast milk.
Disruptions in the breast milk microbiota are a critical concern since they may have a deleterious impact on newborn health and development. Previous research has linked changes in the neonatal microbiome to a variety of chronic diseases, including Crohn’s disease, diabetes mellitus, and obesity. The new study suggests that babies of HIV positive mothers on combined antiretroviral therapy can enjoy the many benefits associated with breast feeding without adverse effects to their microbiome.
Antibiotics are one of the most commonly administered classes of medications to postpartum mothers for a variety of reasons. This pattern can be seen in both emerging and developed countries. In Denmark, for example, more than one-third of women were prescribed at least one medicine after delivery, most of which were antibiotics. According to a survey conducted in India, 90 percent of moms delivering in hospitals, regardless of mode of birth, were prescribed an antibiotic. Antibiotics were given to about the same amount of women who attended postnatal clinics. Antibiotics were prescribed to approximately one in every eight moms who gave birth at home and were followed up on in hospitals.
Globally, children under the age of 15 account for approximately 5% of all HIV-positive people, 10% of new HIV infections, and 15% of all AIDS-related fatalities. Children under the age of one year are among the most vulnerable to HIV. Early antiretroviral medicine administration in HIV-infected neonates has been shown to save lives; yet, coverage of essential intervention among children remains inadequate.





