Proceding with therapy for patients nearing the end of their lives delays discussions about goals of care and hospice enrollment, raises costs, and may have an adverse effect on the quality of care patients receive.Likewise, over the past ten years, significant expert social orders have suggested that clinicians decline the utilization of foundational anti-malignant growth treatments toward the end of life stage.
In a review distributed today in JAMA Oncology, specialists at Yale Malignant Growth Place, in a joint effort with scientists from Flatiron Wellbeing, Inc., uncovered that notwithstanding these proposals, forceful disease care toward the end of life continues and there has been a significant change from the utilization of chemotherapy to immunotherapy.
“Throughout the past ten years, the landscape of fundamental enemy of disease treatment has changed emphatically following the endorsements of different new designated treatments,” said Kerin Adelson, MD, Academic partner of Medication (Clinical Oncology), Boss Quality Official and Vice President Clinical Official for Smilow Malignant Growth Emergency Clinic, and senior author on the review.
“The quality measure that was created a decade prior by proficient oncology associations, centers around decreasing end-of-life chemotherapy fully intent on furnishing patients with prior palliative consideration. It is unclear whether this has helped the end of life care patients get. “
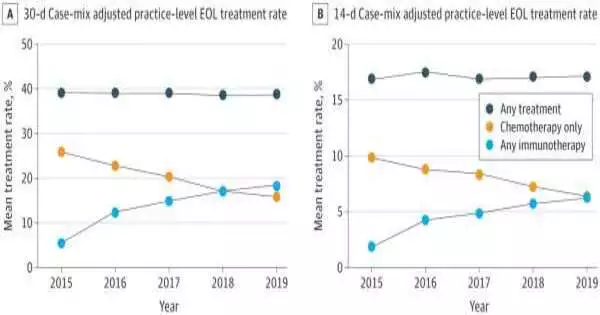
To find out more, the specialists utilized the cross-country Flatiron Wellbeing electronic well being record (EHR)-inferred data set to assess grown-up patients with malignant growth who got treatment and kicked the bucket in somewhere around four years of analysis. Over the review period, the pace of therapy in something like 30 days of death among all malignant growth types consolidated didn’t change (39% in 2015 and 2019), with comparative patterns seen for treatment in no less than 14 days of death (17% in 2015 and 2019).
However, the type of fundamental treatment has shifted; there have been general decreases in the use of chemotherapy (26% in 2015 and 16% in 2019) and increases in the use of immunotherapy (5% in 2015 and 18% in 2019).These progressions were most observable in cutting edge non-little cell cellular breakdown in the lungs and urothelial malignant growth where expansions in treatment at end-of-life were driven by expanded designated spot inhibitor use.
“Our examination distinguished no distinction in the general utilization of fundamental enemy of malignant growth treatment toward the end of life starting around 2015. “The endorsement of numerous new immunotherapy specialists has induced an extraordinary substitution peculiarity, subbing immunotherapy for chemotherapy,” said Dr. Adelson. “Expansions in the utilization of designated treatments might have disrupted our capacity to accomplish prior palliative consideration joining and a decrease in intense consideration usage. More exploration is expected to decide whether this change has impacted the manner in which end-of-life care is given.
More information: Maureen E. Canavan et al, Systemic Anticancer Therapy at the End of Life—Changes in Usage Pattern in the Immunotherapy Era, JAMA Oncology (2022). DOI: 10.1001/jamaoncol.2022.4666
Journal information: JAMA Oncology