Pulses are more straightforward to screen today than at any time in recent memory. Because of smartwatches that can detect a heartbeat, all it takes is a speedy flip of the wrist to really take a look at your heart. In any case, checking the cells liable for pulse is considerably more moving, and it’s urged on specialists to create better approaches to dissect them.
Joseph Wu, M.D., Ph.D., overseer of the Stanford Cardiovascular Organization and teacher of medication and radiology, has contrived another foundational microorganism-determined model of heart tissue that gives knowledge into conditions that harvest up when heart cells thump crazy. Specifically, Wu is concentrating on a state called tachycardia, which expands the pulse and can prompt cardiomyopathy, in which the heart loses its capacity to siphon blood adequately in individuals with, in any case, solid heart structures.
“Tachycardia is most likely surprisingly normal,” said postdoctoral researcher Chengyi Tu, Ph.D., who helped lead the work. “It’s accepted to be underdiagnosed in light of the fact that an expansion in pulse is very normal in various sorts of heart illnesses, and it gets concealed.”
“We can better understand the impact of fast heart rates on our bodies by modeling tachycardia-induced cardiomyopathy with human stem cell-derived heart tissues.”
Wu, the Simon H. Stertzer, M.D., Professor who is the senior author of the study.
To concentrate on tachycardia-prompted cardiomyopathy, the specialists designed heart cells from human immature microorganisms to reveal how our body’s motor runs when it’s in overdrive.
“Displaying tachycardia-prompted cardiomyopathy with human undifferentiated cell-inferred heart tissues permits us to more readily comprehend the effect of quick pulses on our bodies,” said Wu, the Simon H. Stertzer, M.D., teacher who is the senior creator of the review. It was distributed on November 27 in Nature Biomedical Designing. Tu is the lead creator.
Designing heart cells
Dissimilar to most kinds of organ tissues, heart cells are very challenging to fill in a lab. Patient heart cells refined in a dish watch out for de-separate or lose their essential capability and neglect to thump.
Tu stated, “Ideally, you want to take samples of a patient’s heart right after the disease has been diagnosed, while the patient is ill, and after treatment.” You need a lot of replicates to give you statistical power to validate your discovery, but clinically, it is impossible to sample so frequently.”
Given the shortage of tissue, Wu and his partners developed in excess of 400 heart tissue tests from foundational microorganisms to take a gander at the capabilities of heart cells, a cycle that spanned over four years.
“Making designed heart tissue is totally different from making refined cells in a dish. The course of events is extremely lengthy,” Tu said. It takes approximately two weeks to generate heart cells from stem cells; assembling them in a 3D tissue and developing them requires nearly two months.
Reestablishing the compound equilibrium
Utilizing a wired chamber, the scientists electrically invigorated the phones, initiating tachycardia. They tried to determine whether the cells could recover from tachycardia throughout the span of 10 days. During the initial five days, the phones’ capacity to contract persistently declined to around half of their ordinary capability. Yet, when the scientists halted the electrical feeling, the cells made a full recovery in five days.
This is consistent with what medical professionals already know about tachycardia-induced cardiomyopathy, which is largely reversible. At the point when an individual’s pulse dials back, their heart tissue capability gets back to business as usual.
In another examination, scientists prompted tachycardia in an alternate gathering of designed heart tissue. Then, at that point, in the wake of halting excitement, the group enhanced the tissues with NAD—a particle that upholds energy responses—and saw the heart cells’ capability recuperate all the more quickly. The enhanced tissues had recovered 83% of their unique capability by the primary day, while the untreated gathering showed little improvement.
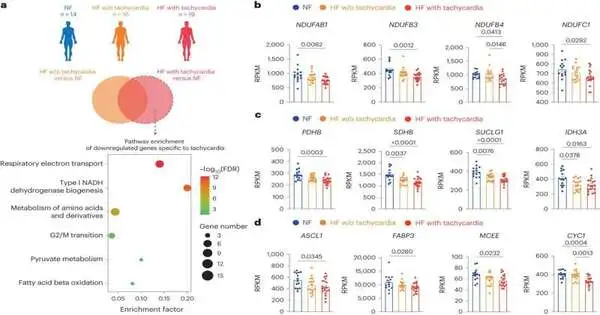
To approve their discoveries, the group contrasted the designed heart tissues with clinical human information and canine model information. “I was astonished by how well the designed heart tissues mirror the genuine human hearts,” Tu said.
Uncovering the molecular switch In tachycardia, the fast heart rate prevents the heart’s chambers from fully filling and contracting, making it difficult for the heart to pump blood to the rest of the body. Assuming it continues for a few days or weeks, which can occur in extreme cases, the veins stop providing sufficient oxygen to the heart tissue and the remainder of the body.
The heart uses fat for energy when it beats normally, but breaking down fats requires a lot of oxygen. In a process known as metabolic rewiring, the heart’s fuel source changes to sugar when it doesn’t have oxygen. The fuel switch and hypoxia, or absence of oxygen, add to a decline in the NAD/NADH proportion, a crucial compound couple that keeps up with the capability of a protein in heart tissue known as SERCA.
“Changing levels of the SERCA protein behave like a gas and brake pedal for a vehicle,” Tu said. At the point when scientists increment how much NAD, the heart’s gas pedal is pushed, and the SERCA protein reinforces the heartbeat of the designed cells. At the point when they are diminished, the designed heart tissues hit the brakes, making them thump all the more pitifully.
By giving patients NAD through an off-the-rack supplement or by IV infusion, clinicians accept they can reestablish the compound equilibrium and speed up a patient’s recuperation.
Close by another conceivable enhancement to assist patients with recuperating from tachycardia, the examination shows the significance of new strategies to demonstrate sickness. Last year, President Joe Biden signed the FDA Modernization Act 2.0 into law, which eliminated the necessity for creature testing before human medication preliminaries.
“Presently, there is more requirement for non-creature models to supplement the creature models,” Tu said. “This work demonstrates that it’s feasible to display complex cardiovascular circumstances using a general non-creature model to concentrate on this illness and test potential therapeutics.”
More information: Chengyi Tu et al. Tachycardia-induced metabolic rewiring as a driver of contractile dysfunction, Nature Biomedical Engineering (2023). DOI: 10.1038/s41551-023-01134-x