As per another review from the Garvan Foundation of Clinical Exploration, acquainting microbes with a cancer’s microenvironment creates a condition of intense irritation that sets off the invulnerable framework’s essential responder cells to go after instead of safeguarding a growth.
The cells on call, called neutrophils, are white platelets that assume a significant role in guarding against contamination. While they by and large safeguard against illness, they are famous for advancing cancer development; elevated degrees of them in the blood are ordinarily connected with less fortunate results in malignant growth, to a limited extent since they produce particles that safeguard the growth by smothering different components of the resistant framework.
The analysts, led by Dr. Tatyana Chtanova, head of the Natural and Growth Immunology Lab at Garvan and academic partner at the School of Biotechnology and Biomolecular Sciences at UNSW Sydney, found that infusing inactivated Staphylococcus aureus organisms inside a cancer switched that defensive action, invigorating the neutrophils to obliterate the cancer in a scope of creature disease models, including Lewis lung carcinoma, triple-negative bosom malignant growth, melanoma, and pancreatic malignant growth.
“Microbial treatment, another type of cancer immunotherapy, has been found to be an effective booster for checkpoint inhibitor therapy. We anticipate that this synergistic effect will eventually lead to better treatments for patients with advanced or previously untreatable malignancies.”
Dr. Andrew Yam, clinical medical oncologist at The Kinghorn Cancer Center.
“Utilizing the resistant framework to battle disease has been perhaps the greatest leap forward in malignant growth treatment over the most recent twenty years, yet right now immunotherapy for further developing white blood cell capability doesn’t work for a wide range of malignant growth. We chose to utilize an alternate kind of immunotherapy that targets neutrophils to understand how creating intense irritation in the immunosuppressive cancer microenvironment influences results,” says Dr. Chtanova.
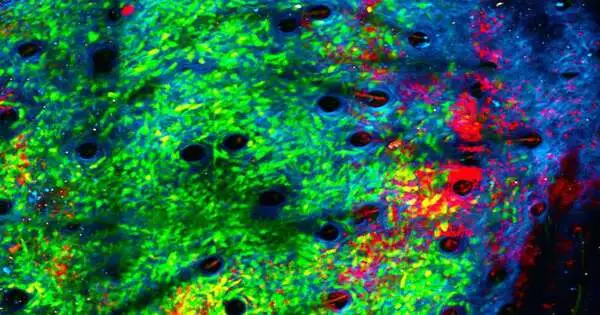
The group utilized intravital imaging in creature studies to see inside the cancers continuously.
“Since going after microbes is the justification behind neutrophils’ presence, we had a decent suspicion that acquainting microorganisms would carry neutrophils to the site and enact them. We found that it’s exceptionally viable in inspiring them to kill the growths, biting up their lattice,” she says.
The review, distributed in the journal Disease Exploration, shows that the neutrophils additionally change at the quality articulation level: they start to discharge particles that will draw in contender white blood cells as support.
“We’ve shown that microbial treatment is a viable supporter for designated spot inhibitor treatment, one more kind of malignant growth immunotherapy. We trust this synergistic impact will at last prompt better therapies to further develop results for patients with cutting-edge or already untreatable malignant growths,” says the first author of the review, Dr. Andrew Sweet Potato, clinical oncologist at The Kinghorn Disease Center and Ph.D. understudy at Garvan.
The review zeroed in on essential growths. Over the course of the following three to five years, the group will foster the treatment to battle metastasis, the spread of malignant growth to different regions of the body, with clinical preliminaries to follow.
More information: Andrew O. Yam et al, Neutrophil conversion to a tumor-killing phenotype underpins effective microbial therapy, Cancer Research (2023). DOI: 10.1158/0008-5472.CAN-21-4025