Fluorescent sensors, which can be utilized to mark and picture a wide assortment of particles, offer a remarkable look inside living cells. They must, however, be used in cells filled in a lab dish or in tissues near the body’s outer layer because their signal is lost when they are embedded too deeply.
MIT engineers have now concocted a method for beating that limit. Using a novel photonic method they created for invigorating any fluorescent sensor, they had the option to further develop the fluorescent sign decisively. With this methodology, the specialists showed they could embed sensors as deep as 5.5 centimeters in tissue and still get areas of strength for a
According to the researchers, this type of technology could allow fluorescent sensors to be used to track specific atoms within the brain or other deep tissues within the body for clinical determination or to test drug effects.
“If you have a fluorescence sensor that can probe biochemical information in cell culture or thin tissue layers, this method allows you to transfer all of those fluorescent dyes and probes into thick tissue.”
Volodymyr Koman, an MIT research scientist
“In the event that you have a fluorescent sensor that can test biochemical data in cell culture or in dainty tissue layers, this innovation permits you to decipher those fluorescent colors and test into thick tissue,” says Volodymyr Koman, a MIT research researcher and one of the lead creators of the new review.
Naveed Bakh SM ’15, Ph.D. ’20 is likewise a lead creator of the paper, which shows up today in Nature Nanotechnology. Michael Strano, the Carbon P. Dubbs Professor of Chemical Engineering at MIT, is the senior creator of the review.
Upgraded fluorescence
Researchers utilize a wide range of sorts of fluorescent sensors, including quantum dabs, carbon nanotubes, and fluorescent proteins, to name a few particles inside cells. By focusing laser light on them, their fluorescence should be visible. In any case, this doesn’t work in thick, thick tissue or profound inside tissue, since tissue itself likewise transmits some bright light. This light, called autofluorescence, muffles the signal coming from the sensor.
“All tissues auto fluoresce, and this turns into a restricting variable,” Koman says. “As the signal from the sensor becomes more vulnerable and more fragile, it becomes surpassed by the tissue autofluorescence.”

To overcome this limit, the MIT group concocted a method for tweaking the recurrence of the bright light produced by the sensor with the goal that it tends to be all the more effectively-recognized from the tissue autofluorescence. Their procedure, which they call frequency-incited recurrence sifting (WIFF), utilizes three lasers to make a laser pillar with a swaying frequency.
While this swaying pillar is radiated onto the sensor, it causes the fluorescence transmitted by the sensor to twofold its recurrence. This permits the fluorescent sign to be handily selected from the foundation autofluorescence. Utilizing this framework, the analysts had the option to improve the sensors’ sign-to-commotion proportion by more than 50-crease.
One potential application for this sort of detection is to screen the adequacy of chemotherapy drugs. To show this potential, the scientists zeroed in on glioblastoma, a forceful kind of cerebrovascular disease. Patients with this kind of malignant growth, for the most part, go through a medical procedure to eliminate as much of the cancer as could reasonably be expected, then, at that point, get the chemotherapy drug temozolomide (TMZ) to attempt to dispose of any excess disease cells.
This medication can have serious side effects, and it doesn’t work for all patients, so it would be useful to have an approach to effectively screen regardless of whether it’s working, Strano says.
“We are dealing with innovation to make little sensors that could be embedded close to the actual growth, which can give a sign of how much medication is showing up at the growth and whether it’s being utilized.” “You could put a sensor close to the cancer and confirm from outside the body the viability of the medication in the genuine growth climate,” he says.
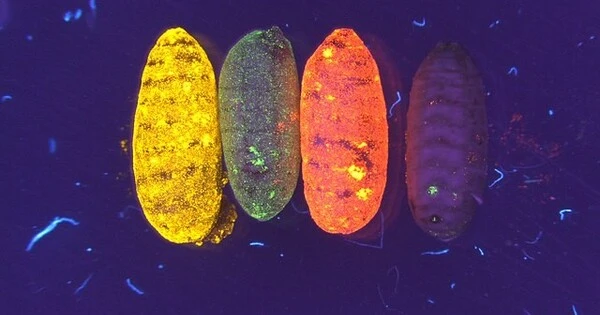
When temozolomide enters the body, it gets separated into more modest mixtures, including one known as AIC. The MIT group planned a sensor that could distinguish AIC and demonstrated the way that they could embed it as profoundly as 5.5 centimeters inside a creature’s cerebrum. They had the option to peruse the sign from the sensor even through the creature’s skull.
Such sensors could likewise be intended to identify sub-atomic marks of cancer cells passing, like reactive oxygen species.
“Any frequency”
As well as identifying TMZ movement, the scientists showed how they could utilize WIFF to upgrade the sign from an assortment of different sensors, including carbon-nanotube-based sensors that Strano’s lab has recently evolved to recognize hydrogen peroxide, riboflavin, and ascorbic acid.
“The procedure works at any frequency, and it tends to be utilized for any fluorescent sensor,” Strano says. “Since you have quite a lot more information now, you can embed a sensor at profundities that were unrealistic previously.”
For this review, the specialists utilized three lasers together to make the wavering laser bar. However, in future work, they desire to utilize a tunable laser to make the sign and further develop the strategy considerably further. The scientists say that this ought to turn out to be more achievable as the cost of tunable lasers diminishes and they become quicker.
To assist with making fluorescent sensors simpler to use in human patients, the specialists are chipping away at sensors that are naturally resorbable, so they would have no need to be precisely taken out.