A ‘bio-artificial’ pancreas created in the lab using placental stem cells, as well as a DIY insulin-monitoring and release system, are being developed to provide people with insulin-dependent diabetes with an alternative to waiting for a pancreas transplant.
The pancreas contains cells that regulate the quantity of sugar in the blood, but for unknown reasons, the immune system periodically targets and kills them. When this happens, a person develops Type 1 diabetes, a condition in which the body loses the ability to generate insulin, the enzyme that transports sugar throughout the body to power important functions.
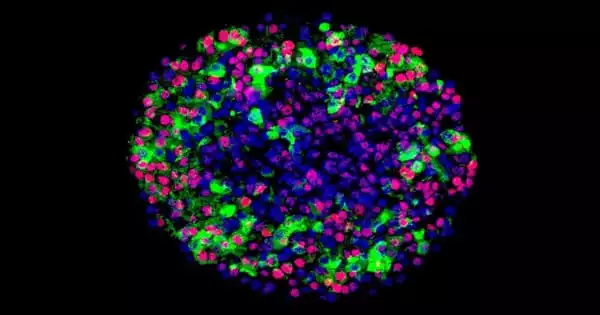
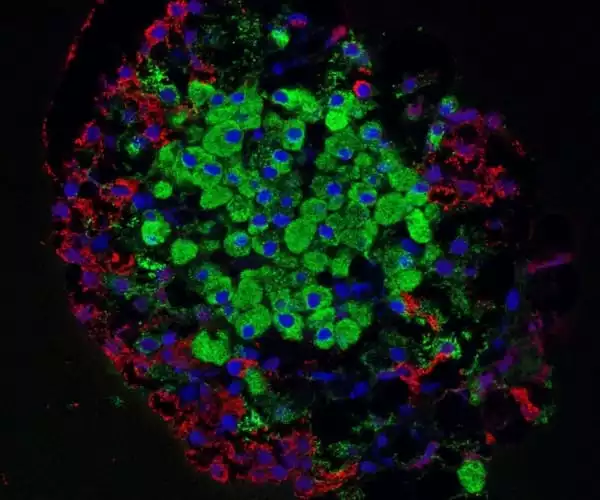
Researchers have made ground-breaking attempts to improve the functionality of pancreatic cells derived from stem cells. The researchers revealed in a new study that stem cells can generate cells that closely resemble normal pancreatic islets in terms of structure and function.
Insulin is a hormone that is produced by pancreatic beta cells. Type 1 diabetes is caused by the loss of these cells, which necessitates many daily insulin injections to compensate for the lost insulin.
Insulin secretion in diabetic individuals can be restored by transplanting beta cells obtained from the pancreas of a brain dead organ donor. However, because cells from at least two donors are required to cure one diabetic, this treatment has not been generally adopted.
In our study, insulin secretion was regulated as usual in cells, and the cells responded to changes in the glucose level even better than the pancreatic islets isolated from organ donors that were used as controls.
Väinö Lithovius
Attempts have been done for a long time to generate functioning beta cells from stem cells, which could make this treatment more widespread. However, so far, beta cells derived from stem cells have been immature, with poorly controlled insulin production. This could explain why no advancements have been made in therapeutic studies based on immature cells now being conducted in the United States.
Professor Timo Otonkoski’s research group at the University of Helsinki has made ground-breaking attempts to improve the functionality of pancreatic cells derived from stem cells.
In a newly published lengthy research, the scientists revealed for the first time that stem cells may create cells that nearly resemble normal pancreatic islets in terms of both structure and function. The work was published in the journal Nature Biotechnology, and it was primarily financed by the Academy of Finland’s Center of Excellence MetaStem.
“In our study, insulin secretion was regulated as usual in cells, and the cells responded to changes in the glucose level even better than the pancreatic islets isolated from organ donors that were used as controls,” says Väinö Lithovius, a member of the research group.
The most comprehensive survey of beta cell function
The researchers demonstrated the function of stem cell-derived beta cells in cell cultures as well as mouse tests. In the latter, the researchers proved that stem cell-derived beta cells implanted into mice began successfully controlling the animals’s glucose metabolism.
“Blood glucose levels in mice are around 8-10 millimolar greater than in humans. Following cell transplantation, the level dropped to around 4-5 millimolar, which is comparable to that reported in humans. It maintained at this level, demonstrating that the stem cell-derived transplant was capable of regulating blood glucose levels in mice “Jonna Saarimäki-Vire, the researcher in charge of the cell transplantation, explains.
The current survey of beta cell function is the most comprehensive in the field: in addition to insulin secretion, the researchers investigated the functionality of systems that regulate insulin secretion, such as metabolism and ion channels, and linked the findings to gene expression during development.
Without a completely functional pancreas, a diabetic risks sustained high blood-glucose levels, which can result in long-term health consequences such as blindness and limb loss, while falling too low can result in fainting or, worse, death. To stay healthy, a person with Type 1 diabetes must inject insulin multiple times each day, as well as constantly check blood glucose levels, which are generally measured through finger prick blood tests.
“Our research will assist to increase the creation of stem cell islets, making it easier to use them in disease modeling and cell therapies,” says Timo Otonkoski. “I believe the international scholarly community appreciates our efforts to verify stem cell islets as instruments for diabetes research and cell therapies,” says Uppsala University Professor Anders Tengholm, who collaborated to the study.