As per a review from specialists at Weill Cornell Medication, neurons that sense torment safeguard the stomach from irritation and related tissue harm by controlling the microbial local area living in the digestion tracts.
The analysts, whose report appeared Oct. 14 in Cell, found in a preclinical model that torment detecting neurons in the stomach discharge an atom called substance P, which seems to safeguard against stomach irritation and related tissue harm by supporting the number of inhabitants of valuable microorganisms in the stomach. The analysts additionally found that these agony-detecting nerves are decreased in number, with huge disturbances to their aggravation-flagging qualities, in individuals who have fiery entrail sickness (IBD).
“These discoveries reshape our pondering constant incendiary illness and open up an entirely different way to deal with restorative intercession,” said senior creator Dr. David Artis, head of the Jill Roberts Establishment for Exploration in Provocative Entrail Sickness, overseer of the Friedman Place for Nourishment and Aggravation, and the Michael Kors Teacher of Immunology at Weill Cornell Medication.
The concentrate’s most memorable creator, Dr. Wen Zhang, a postdoctoral scientist in the Artis research facility, added that “characterizing a formerly obscure tactile capability for these particular neurons in impacting the microbiota adds another degree of understanding to having microbiota communications.”
“The discovery of a previously unknown sensory function for these specific neurons in influencing the microbiota adds a new level of understanding to host-microbiota interactions.”
Dr. Wen Zhang, a postdoctoral researcher in the Artis laboratory,
IBD covers two particular problems, Crohn’s illness and ulcerative colitis, and is accepted to affect a few million individuals in the US. Ordinarily, it is treated with drugs that straightforwardly target components of the safe framework. Researchers currently value that stomach-staying microscopic organisms and different microorganisms additionally assist in directing stomach aggravation.
As Dr. Artis’ research center and others have displayed as of late, the sensory system, which is “wired” into most organs, has all the earmarks of being one more remarkable controller of the insusceptible framework at the body’s boundary surfaces. In the new review, Dr. Artis and his group explicitly analyzed torment neurons that innervate—expand their sensitive spots into—the stomach.
These stomach-innervating torment neurons, whose phone bodies sit in the lower spine, express a surface protein called TRPV1, which fills in as a receptor for torment-related signals. TRPV1 can be activated by high intensity, corrosive, and the stew pepper compound capsaicin, for example, and the cerebrum interprets this enactment as consuming torment.The scientists found that quieting these TRPV1 receptors in stomach nerves, or erasing TRPV1-communicating neurons, prompted a lot of more regrettable irritation and tissue harm in IBD mouse models, while enacting the receptors made a defensive difference.
The examiners saw that the deteriorated irritation and tissue harm in TRPV1-obstructed mice were related to changes in the overall populations of various types of stomach microscopic organisms. When this modified bacterial population was introduced into normal mice, it caused the same level of helplessness, irritation, and harm.Conversely, a wide range of anti-microbial treatments could turn around this weakness even in TRPV1-obstructed mice. This outcome exhibited that TRPV1-communicating nerves safeguard the stomach principally by assisting with keeping a solid stomach microorganism populace.
The researchers found solid proof that a huge piece of this microorganism impacting impact of TRPV1-communicating nerves comes from an atom in the nerve discharge called substance P—which they noticed could invert, all alone, the majority of the destructive impacts of hindering TRPV1. It was additionally recommended that the motion among neurons and microorganisms was two-way — a few bacterial animal types could initiate TRPV1-communicating nerves to inspire them to deliver more substance P.
To affirm the significance to people, the analysts inspected stomach tissue from IBD patients, and found strange TRPV1 and substance P quality movement as well as fewer indications of TRPV1 nerves generally.
“These patients had upset torment detecting nerves, which might have added to their ongoing aggravation,” Dr. Zhang said.
How substance P exerts its effects on the stomach microorganism population and how these organisms “argue” are questions that researchers are currently attempting to answer in ongoing tests.However, the outcomes so far suggest that the up and coming age of calming drugs for IBD and different issues could intensify that focus on the sensory system.
“A ton of current mitigating drugs work in just a few patients, and pharma organizations truly haven’t known why,” Dr. Artis says. Perhaps this is on the grounds that, with regards to constant aggravation, we’ve been seeing just a portion of the image — and presently the rest, including the job of the sensory system, is beginning to come into
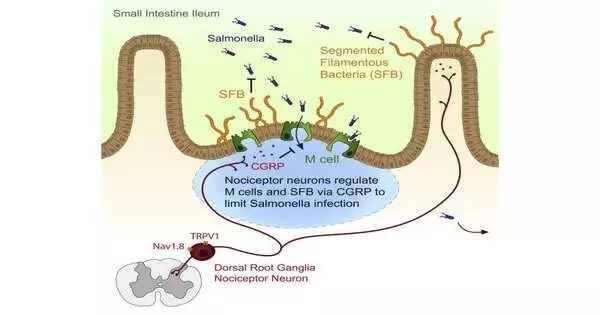
More information: Nicole Y. Lai et al, Gut-Innervating Nociceptor Neurons Regulate Peyer’s Patch Microfold Cells and SFB Levels to Mediate Salmonella Host Defense, Cell (2019). DOI: 10.1016/j.cell.2019.11.014
Journal information: Cell