Humans and other tetrapods have small endocrine glands in their necks called parathyroid glands. Humans typically have four parathyroid glands, which are located in various locations on the back of the thyroid gland. In response to low blood calcium, the parathyroid gland produces and secretes parathyroid hormone, which plays an important role in regulating the amount of calcium in the blood and bones.
A study published in the journal Stem Cell Reports suggests that patient-derived parathyroid organoids (PTOs) could pave the way for future physiology studies and drug-screening applications.
“We are the first group in the world that was able to isolate parathyroid stem cells and maintain these cells in our lab as organoids for an extended period of time,” says co-senior study author Schelto Kruijff of the University Medical Center Groningen. “Our research introduces the PTO as a new model for research on parathyroid diseases.”
Parathyroid diseases are characterized by changes in parathyroid hormone excretion, which results in abnormal blood calcium concentrations. In vitro models could aid in the development of parathyroid-targeted treatments and imaging tracers. Organoids are 3D structures that develop from stem cells and closely mimic tissue architecture and cellular composition. These models have proven to be extremely useful for studying tumor behavior and evaluating drug responses, as well as providing a platform for long-term in vitro experimentation.
We discovered that the parathyroid gland contains stem cells capable of producing organoids. These organoids mimic the patient’s condition, can produce hormones, express specific markers, and have comparable drug reactions.
Schelto Kruijff
“We discovered that the parathyroid gland contains stem cells capable of producing organoids. These organoids mimic the patient’s condition, can produce hormones, express specific markers, and have comparable drug reactions” Kruijff explains.
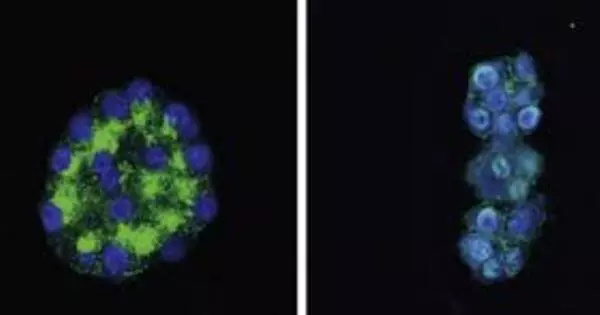
Kruijff and co-senior study author Rob Coppes of the University Medical Center Groningen set out to create a patient-derived PTO model of human parathyroid tissue in this study. Human benign hyperplastic parathyroid tissue was obtained from patients undergoing parathyroid surgery by the researchers. They isolated parathyroid stem cells from tissue and tested their ability to grow and form PTOs.
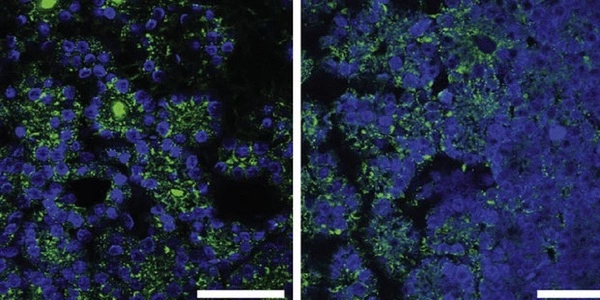
The PTOs matched the original tissue in terms of gene and protein expression as well as functionality. Additional findings revealed increased and decreased hormone secretion in response to calcium concentration changes and parathyroid hormone-lowering drugs. Furthermore, the researchers discovered specific parathyroid-targeted tracer uptake in PTOs. The findings show that these organoids have the potential to mimic human parathyroid function.
One study limitation was the absence of the original microenvironment, which included blood vessels and fluctuating extracellular signal concentrations. Nonetheless, the functional testing and tracer experiment demonstrated that PTOs are an excellent model that closely resembles functional parathyroid tissue.
In the future, the researchers intend to transplant these organoids into hypoparathyroid rats to study their function in a living animal model. “Future parathyroid-targeted drugs and imaging tracers can be tested using these organoids. When using organoids, less animal testing is required” Kruijff claims. “This technique could also be used to try to culture healthy parathyroid gland organoids in order to treat hypoparathyroid patients.”