According to research reported in the Lancet Neurology journal, a method that recognizes the accumulation of abnormal protein deposits connected to Parkinson’s disease may help with early detection and be crucial in the clinical diagnosis and characterization of the condition.
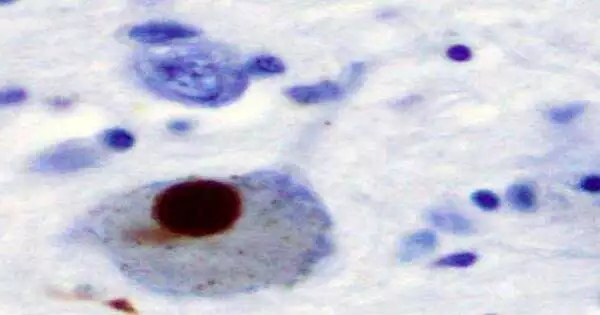
The study’s results show that the method, called the synuclein seed amplification assay (Syn-SAA), is reliable for identifying those who have the neurodegenerative disease and that it may also be able to recognize those who are at risk and those who have non-motor symptoms that first appear before motor symptoms. Parkinson’s disease is characterized pathologically by the presence of misfolded synuclein protein aggregates in the brain.
The University of Pennsylvania Perelman School of Medicine’s co-lead author is Professor Andrew Siderowf, S. “Recognizing heterogeneity in underlying pathology among patients with Parkinson’s disease has been a major challenge,” says Dr. Chen, who is also an investigator for the Parkinson Progression Marker Initiative (PPMI). Finding a reliable biomarker for Parkinson’s disease pathology could have a significant impact on how we treat the condition. It may be possible to diagnose patients earlier, determine the most effective treatments for various patient subgroups, and accelerate clinical trials.
“Recognizing heterogeneity in underlying pathology among Parkinson’s disease patients has been a major challenge.” Finding an effective biomarker for Parkinson’s disease pathology could have far-reaching ramifications for how we treat the disease, perhaps allowing us to diagnose patients sooner, identify the best treatments for diverse subsets of patients, and accelerate clinical trials.”
Professor Andrew Siderowf, of the University of Pennsylvania Perelman School of Medicine (U.S.).
“Our results indicate that the Syn-SAA technique is highly sensitive to the biomarker for Parkinson’s disease regardless of the clinical features, making it possible to accurately diagnose the disease in patients at an early stage. Additionally, our findings show that misfolded synuclein is detectable prior to the onset of imaging-detected dopaminergic damage in the brain, suggesting widespread spread of these misfolded proteins prior to significant neuronal damage,” continues study co-lead author Luis Concha, director of research and development at Amprion (U. S.).
The new study offers the most comprehensive examination of Syn-SAA’s abilities as a Parkinson’s disease diagnostic tool. A large-scale study with such a wide range of carefully described participants has never before been carried out, despite prior research showing that Syn-SAA can clearly distinguish between people with Parkinson’s disease and those without the condition.
Using information from the Parkinson’s Progression Markers Initiative (PPMI) cohort, the authors evaluated the value of Syn-SAA for identifying underlying heterogeneity in people with Parkinson’s disease and its capacity to identify early signs of the condition. Parkinson’s disease diagnoses and at-risk individuals with gene variants (GBA and LRRK2) linked to the condition were included among the 1,123 participants in the analysis.
Participants who were considered prodromal were also included. These individuals had non-motor symptoms like disturbed sleep or a loss of smell, which can be early indicators of Parkinson’s disease, but they were undiagnosed and lacked any of the typical motor symptoms like tremors or muscle stiffness, which typically appear later in the course of the disease. To find out if Syn-SAA could predict Parkinson’s onset and aid in the diagnosis of those who already have symptoms, it was decided to include prodromal participants.
Each participant provided samples of the cerebrospinal fluid, which surrounds the brain and spinal cord. With the aid of this ground-breaking method, minute quantities of misfolded synuclein aggregates can now be detected using conventional laboratory procedures.
The analyses’ results show that Syn-SAA accurately diagnoses Parkinson’s disease in 88 percent of participants who have received a diagnosis (combining sporadic and genetic cases).
93% of people had a positive Syn-SAA result in sporadic cases—those without a known genetic cause. A positive Syn-SAA was found in 96% of those with the GBA variant, compared to a positive Syn-SAA in 68% of those with LRRK2, for those with genetic forms of Parkinson’s disease.
Even though they had not yet received a Parkinson’s disease diagnosis, the majority of prodromal participants had positive synuclein aggregate results from the Syn-SAA test. 16 of the 18 participants who were selected for the study based on their loss of smell had positive Syn-SAA results, or 89 percent of the group. Similar to this, positive Syn-SAA results were found in 85% (28/33) of cases in people with REM sleep behavior disorder, a sleep disorder that is known to be an early sign of Parkinson’s disease. A positive Syn-SAA result was not linked to any additional clinical characteristics.
Non-manifesting carriers (NMCs), or individuals who carried LRRK2 or GBA variants but did not have a Parkinson’s disease diagnosis or prodromal symptoms, had positive Syn-SAA results in 9% (14/159) and 7% (11/151), respectively, of participants.
Importantly, brain scans of the majority of prodromal participants and NMCs with positive Syn-SAA did not reveal a decrease in the anticipated number of dopamine-producing nerve cells, which is a biomarker signature that is present even before diagnosis. According to this finding, the accumulation of synuclein aggregates may serve as a very early sign of the onset of a disease.
Loss of smell, one of the most typical symptoms in prodromal individuals and those with a Parkinson’s disease diagnosis, was the clinical feature that most strongly predicted a positive Syn-SAA result. In comparison to the 63% of Parkinson’s disease participants whose sense of smell was unaffected, 97 percent of participants with loss of smell had positive Syn-SAAs.
This study found people with positive Syn-SAA results who had not yet lost their sense of smell, indicating that synuclein pathology may be present even before there is a measurable loss of sense of smell. Loss of smell does appear to be a strong predictor of Parkinson’s disease, but it’s important to note that this study also found people who had not yet lost their sense of smell. Further studies are required to determine how patients’ sense of smell may change over time and how this may relate to the accumulation of a-synuclein aggregates in the brain, according to study author Dr. Tanya Simuni of Northwestern University (U.S.).
Age and sex differences in Syn-SAA results were also observed, especially in those with a mutation in LRRK2. While 79 percent of male participants with an LRRK2 variant and Parkinson’s disease had positive Syn-SAA results, only 55 percent of female participants did. Negative Syn-SAA results were also associated with an increased likelihood of being older (69 vs. 62 years) than those who had favorable Syn-SAA outcomes. The outcomes showed no gender differences in patients with sporadic or GBA-associated Parkinson’s disease.
15 participants with a history of Parkinson’s disease were autopsied; 14 of them had typical pathology and tested positive for Syn-SAA. The only person with a negative Syn-SAA result also had a LRRK2 variant, but their sense of smell was unaffected in life.
The authors are aware that their study has some limitations. By addressing problems caused by variables like skewed data and low sample sizes for some participant groups, more samples would enhance analyses. The analyses that have been provided are all cross-sectional, but future research could evaluate changes over specific time periods if PPMI samples that have been collected over time are made available. Further research into variations in Syn-SAA results between people with various genetic forms of Parkinson’s disease is also required, as are longer-term studies.
Professors Daniela Berg and Christine Klein from the University Hospital Schleswig-Holstein in Germany, who were not involved in the study, emphasized the importance of the finding that abnormal -synuclein aggregation could detect early signs of disease in a linked Comment: “Siderowf and colleagues showed that people with prodromal Parkinson’s disease and non-manifesting mutation carriers had abnormal -synuclein aggregation before any other detectable clinical or….
Although the blood-based method needs to be further elaborated for scalability, Berg and Klein assert that Syn-SAA is a game-changer in Parkinson’s disease diagnostics, research, and treatment trials. Blood tests will be necessary to fully utilize Syn-SAA’s potential.
More information: Assessment of heterogeneity among participants in the Parkinson’s Progression Markers Initiative cohort using α-synuclein seed amplification: a cross-sectional study, The Lancet Neurology (2023). www.thelancet.com/journals/lan … (23)00109-6/fulltext