Safe cells assume a functioning and cozy role in coordinating the development of human lung tissue during improvement, scientists find, upsetting our comprehension of how we might interpret early lung advancement and the job of resistant cells beyond invulnerability.
The examination offers new experiences for understanding and treating respiratory circumstances, like ongoing obstructive aspiratory infection (COPD). Nearly 20% of all deaths involving children under the age of five worldwide are caused by respiratory conditions.
The work uncovers amazing coordination between the safe and respiratory frameworks, significantly sooner being developed than recently suspected. This disclosure brings up issues about the likely job of resistant cells in other organs across the body.
Specialists from the Wellcome Sanger Establishment, College School London (UCL), and their teammates at EMBL’s European Bioinformatics Foundation utilized progressed single-cell innovations to plan the advancement of early human lung-safe cells after some time.
“By using a targeted approach to mapping the immune system, we discovered a symbiotic relationship between immune cells and developing lungs. These thorough findings pave the way for new regeneration therapies not only in the lung, but also in other critical human organs.”
Dr. Peng He and Dr. Jo Barnes, co-first authors of the study at the Wellcome Sanger Institute
This study has made a first-of-its-sort safe cell map book of the creating lung. It is a component of the global Human Cell Atlas project, which is mapping every type of human cell to improve our comprehension of health, infection, and disease.
The mechanisms underlying childhood lung diseases will be better understood thanks to the findings, which were published in Science Immunology.
Immunohistochemistry showing spatial appropriation of resistant cells in 9 pcw fetal lungs (covered utilizing Imaris programming). Credit: Josephine L. Barnes
Immune cells make up a lot of the airways and mature lungs. These immune cells play important roles in gas exchange and protecting the respiratory tract from infection. In contrast to structural or lining cell types, the roles of immune cells in the developing organ have not been investigated. The presence of immune cells in human lungs as early as five weeks into development has been confirmed by recent discoveries.
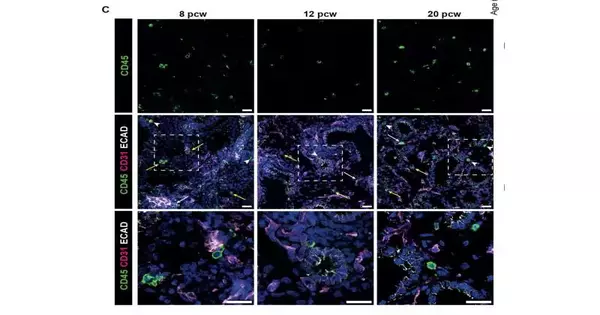
To investigate whether the safe framework could impact how lungs develop, the group concentrated on resistant cells in early human lungs from 5 to 22 weeks of improvement. They utilized different methods, including single-cell sequencing, and explored different avenues regarding lung cell societies to check whether insusceptible cells could influence lung cell advancement.
They recognized key controllers of lung advancement, including flagging atoms IL-1β and IL-13 that work with the coordination of lung immature microorganisms separating into particular mature cell types.
The researchers observed an infiltration of innate immune cells, followed by an adaptive immune cell infiltration. Natural killer (NK) cells, innate lymphoid cells (ILCs), myeloid cells, and progenitor cells are examples of innate cells. Concerning versatile resistant cells as well as lymphocytes, both creating and mature B heredity cells were identified, demonstrating that the lung climate upholds B cell improvement.
The findings fundamentally alter our comprehension of the immune and epithelial interactions necessary for the maturation of the fetal lung. They likewise recommend that early invulnerable unsettling influences could appear as pediatric lung infections.
These new experiences into systems in early lung arrangement will likewise add to the advancement of new helpful methodologies for recovering harmed lung tissue and reestablishing lung capability.
“By adopting a focused strategy for mapping the immune system, we reveal a symbiotic relationship between immune cells and developing lungs,” stated Dr. Peng. He and Dr. Jo Barnes are co-first authors of the study from the Wellcome Sanger Institute, EMBL’s European Bioinformatics Institute, and the UCL Division of Medicine, respectively. These itemized experiences pave the way for likely regenerative treatments in the lung, however, in other essential human organs.”
Dr. Marko Nikolić, senior creator of the review at the UCL Division of Medication and privileged specialist in respiratory medication, said, “We currently realize resistant epithelial crosstalk is a component of early lung improvement. Understanding what happens when lung developmental processes are disrupted, such as in preterm births, which can result in respiratory deficiencies, will be made easier with this crucial baseline of healthy lung development.
“The active participation of immune cells expands the possibilities for understanding and addressing impaired lung formation,” said senior author Dr. Kerstin Meyer at the Wellcome Sanger Institute. What is really thrilling about this component is that it might well apply in other organ frameworks as well.”
Dr. Sarah Teichmann, senior creator of the review at the Wellcome Sanger Organization and Prime supporter of the Human Cell Chart book, said, “In the event that we are to completely comprehend the underlying drivers of sickness, we require a total perspective on cells at all stages in the human body. The study of lung diseases will greatly benefit from this significant contribution to a comprehensive human cell Atlas.”
More information: Josephine Barnes et al, Early human lung immune cell development and its role in epithelial cell fate, Science Immunology (2023). DOI: 10.1126/sciimmunol.adf9988. www.science.org/doi/10.1126/sciimmunol.adf9988