A healthy microbiome may shield critically ill patients from life-threatening infections, according to a University of Calgary study. The investigation focused on how the immune system and the human gut interact. Results demonstrated that the gut microbiota and systemic immunity function as a dynamic “metasystem,” in which issues with the gut microbes and immune system dysfunction are related to significantly higher rates of hospital-acquired infections.
The results imply that we cannot simply target these harmful bacteria and the immune system separately if we want to fight infection. According to the researchers, an all-encompassing perspective of how things are operating is required.
Between 20 and 50 percent of all critically ill patients develop potentially fatal infections while receiving intensive care or after leaving the ICU, significantly raising the risk of death.
“Despite the use of antibiotics, hospital-acquired infections remain a major clinical concern for which there are no acceptable answers. We approached this problem from a different perspective. We investigated the body’s natural defense against infection in order to better understand why some people are more vulnerable to these devastating diseases.”
Dr. Braedon McDonald, MD, Ph.D., an intensive care physician at the Foothills Medical Centre (FMC).
Hospital-acquired infections continue to be a significant clinical problem despite the use of antibiotics, for which there are no effective treatments, according to Dr. Braedon McDonald, MD, Ph.D., an assistant professor at the Cumming School of Medicine (CSM) and an intensive care physician at the Foothills Medical Centre (FMC). “We took a different approach to this problem. To better understand why some people are more vulnerable to these deadly infections, we took a closer look at the body’s natural defense against infection.”.
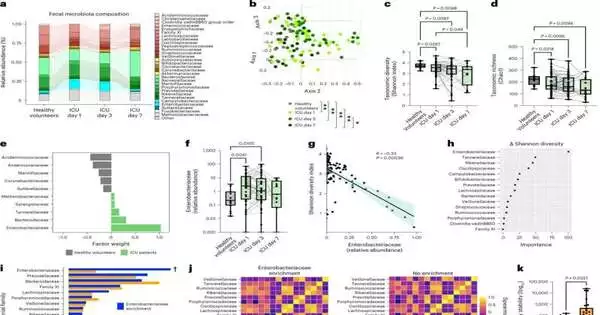
51 patients who had just been admitted to the FMC intensive care unit (ICU) participated in the study. During the first week of an acute critical illness, patients were observed. According to research, the gut microbiota and systemic immunity function as a dynamic “metasystem,” and issues with the gut microbiota and immune system are linked to significantly higher rates of hospital-acquired infections.
According to research, a family of bacteria that naturally exist in the gut appears to be significant for controlling the immune system, according to Jared Schlechte, a Ph.D. candidate in McDonald’s lab and the study’s lead author. “However, when a person is critically ill, the microbiome is damaged, which allows these bacteria to begin dominating.”.
According to the study, which was published in Nature Medicine, patients who experienced a bloom, or abnormal growth, of this common bacteria were most at risk of developing serious infections.
The importance of this information, according to McDonald, lies in the fact that it opens up a whole new line of inquiry into potential preventative measures in addition to infection-fighting strategies. The results indicate that if we want to fight infection, we can’t just target these bad bacteria and the immune system separately. We must adopt a more comprehensive perspective of how things work.”.
As a next step, McDonald and the team intend to start a randomized, controlled clinical trial based on a precision medicine strategy that borrows from probiotic therapy and makes use of numerous different bacteria that have been engineered to specifically target the bacteria found in the study. Engineered microbiomes will be administered to those who consent to participate.
What we’re attempting to do, according to McDonald, is restore the normal mechanisms that operate when we’re healthy and use them to our advantage in order to help protect people from infections.
More information: Jared Schlechte et al, Dysbiosis of a microbiota–immune metasystem in critical illness is associated with nosocomial infections, Nature Medicine (2023). DOI: 10.1038/s41591-023-02243-5