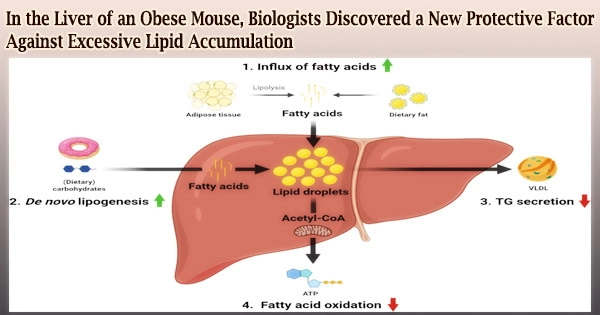
NAFLD (non-alcoholic fatty liver disease), often known as fatty liver disease, is a common illness that affects obese persons. High-fat level in the liver is harmful since it is linked to serious health issues such as diabetes, high blood pressure, and liver cancer.
A study team lead by Dr. Chi Bun CHAN, Assistant Professor at the University of Hong Kong’s (HKU) School of Biological Sciences, Faculty of Science, has discovered a new protective mechanism against this illness.
The outcomes of the study were recently published in the professional journal Hepatology. The liver is a crucial organ that controls the human body’s overall glucose and fat metabolisms.
Hyperglycemia and hyperlipidemia, which are substantial risk factors for diabetes, hyperlipidemia, and liver cancer, will eventually occur from disruption of fat metabolism in the liver.
The number of people with NAFLD is expected to rise from 80 million in 2015 to 100 million by 2030. While the consequences of fat accumulation in the liver have been well documented, it is unknown whether the liver has any protective mechanisms in place to counteract the harm.
Dr. Chan’s team investigated gene expression in the liver of obese mice caused by a high-fat diet and discovered that a protein called SH3 domain binding kinase (SBK1) was selectively enhanced in the obese mouse liver.
We are very excited to see that increasing its activity effectively alleviates the health problems caused by fatty liver. But we still need more studies to fully depict its functional activity so that we can develop SBK1 activator as a new treatment agent for this common liver disease.
Dr. Chi Bun CHAN
SBK1 is a protein kinase that was first found in 2001, but no further research into its functions in mammals has been done. As a result, the activities of this new protein are unknown.
Dr. Chan’s team discovered for the first time that fatty acid buildup in the mouse liver induces SBK1. They also discovered that animals lacking the SBK1 gene in their liver, referred to as ‘LSKO (liver-specific SBK1 knockout) mice,’ have more lipid buildup and fibrosis in this organ.
Furthermore, the LSKO mice had unregulated hepatic glucose output and higher blood glucose levels, as well as being less susceptible to insulin stimulation than the control group, all of which are strong markers of diabetes development.
Dr. Chan’s team used cultured cell models in addition to animal research to figure out how the SBK1 gene controlled lipid metabolism in the liver. They discovered that SBK1 phosphorylated and increased the activity of Nur77, a well-known transcriptional factor that regulates fatty acid absorption and lipid synthesis in liver cells.
When the activity of the SBK1 protein in liver cells was reduced, the cells took up more fatty acids and generated excessive lipid buildup, which interfered with insulin signaling.
Surprisingly, when the SBK1 protein was removed from the cultured liver cells and the LSKO animals, another metabolic hormone in the liver cells, fibroblast growth factor 21 (FGF21), was also reduced.
Because FGF21 is a key hormone that allows the liver to communicate with other peripheral organs such white adipose tissues, decreased FGF21 hormone synthesis in the LSKO liver disrupts this communication, leading to the development of insulin resistance in other tissues.
The researchers wanted to see if altering the SBK1 protein activity in the liver could help reverse the harmful effects of obesity.
They transiently enhanced the amount of SBK1 protein in the mouse liver with fructose diet-induced fatty liver disease and observed pathological signs such as liver steatosis, inflammation, and so on using adenovirus-mediated gene delivery. Hyperlipidemia, hyperglycemia, and hypertension were all reduced.
“Our findings clearly show that SBK1 protein is an important regulator of the lipid metabolism that was neglected before,” said Dr. Chan.
“We are very excited to see that increasing its activity effectively alleviates the health problems caused by fatty liver. But we still need more studies to fully depict its functional activity so that we can develop SBK1 activator as a new treatment agent for this common liver disease,” Dr. Chan further added.
The Hong Kong Research Grant Council, the Health and Medical Research Fund, and HKU Seed Fund for Basic Research supported this work.
Key findings on the liver protective factor SBK1:
- Fatty acid accumulation causes the mouse liver to produce the SBK1 protein, which regulates lipid accumulation and fibrosis.
- In liver cells, the SBK1 protein phosphorylates and promotes the activity of Nur77, a well-known transcriptional factor that regulates the expression of genes involved in lipid production. When SBK1 activity is reduced, Nur77-controlled gene expression is disrupted, resulting in increased fatty acid absorption and lipid buildup.
- Inadequate SBK1 protein reduces the synthesis of the metabolic hormone fibroblast growth factor 21 (FGF21) in liver cells, impairing communication between the liver and other organs and leading to insulin resistance in other tissues.