According to a new study, rejuvenating immune cells that live in tissues surrounding the brain improves fluid flow and waste clearance from the brain and may help treat or even prevent neurodegenerative diseases like Alzheimer’s and Parkinson’s.
Alzheimer’s, Parkinson’s, and many other neurodegenerative diseases are characterized by protein clusters that cause damage in the brain. Scientists have worked tirelessly to find ways to treat such conditions by removing toxic clusters, but they have had limited success.
Researchers at Washington University School of Medicine in St. Louis have discovered a novel way to improve waste clearance from the brain, potentially treating or even preventing neurodegenerative diseases. They discovered that the immune cells that surround the brain influence how efficiently waste is swept out of the brain, and that these immune cells are impaired in old mice, as well as in people and mice with Alzheimer’s disease. They also discovered that injecting an immune-stimulating compound into old mice rejuvenates immune cells and improves waste clearance from the brain.
The findings, which were published in Nature, point to a novel approach to reversing some of the effects of aging on the brain.
“Alzheimer’s has been studied for many years from the perspective of how neurons die, but there are other cells, such as immune cells on the periphery of the brain, that also may play a role in Alzheimer’s,” said senior author Jonathan Kipnis, PhD, the Alan A. and Edith L. Wolff Distinguished Professor of Pathology & Immunology and a BJC Investigator.
Our findings suggest that parenchymal border macrophages could potentially be targeted pharmacologically to alleviate brain clearance deficits associated with aging and Alzheimer’s disease.
Jonathan Kipnis
“It doesn’t look likely that we will be able to revive dead or dying neurons, but the immune cells that sit on the borders of the brain are a feasible target for treating age-related brain diseases. They’re more accessible, and could be drugged or replaced. In this study, we treated aged mice with a molecule that can activate aged immune cells, and it worked in improving fluid flow and waste clearance from the brain. This holds promise as an approach to treating neurodegenerative diseases.”
Kipnis is a leading expert in neuroimmunology, the study of how the immune system affects the brain in health and disease. He discovered a network of vessels in 2015 that drains fluid, immune cells, and small molecules from the brain into lymph nodes, which house many immune system cells. He and colleagues demonstrated last year that some investigational Alzheimer’s therapies are more effective in mice when combined with a treatment aimed at improving the drainage of fluid and debris from the brain.
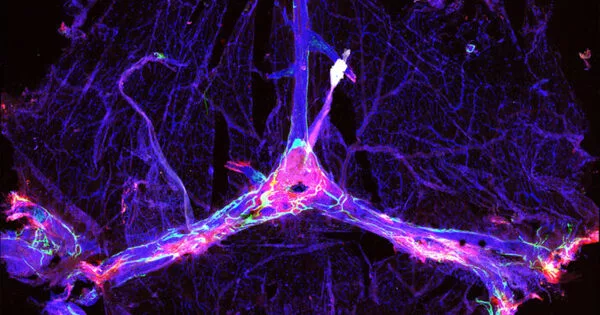
For this study, Kipnis and Antoine Drieu, Ph.D. – a postdoctoral researcher and the paper’s lead author – set out to understand the role played by the immune cells that live along the brain’s vasculature and in the leptomeninges, the tissues immediately surrounding the brain and spinal cord. They termed these cells parenchymal border macrophages, because they sit at the interface between cerebrospinal fluid and brain tissue.
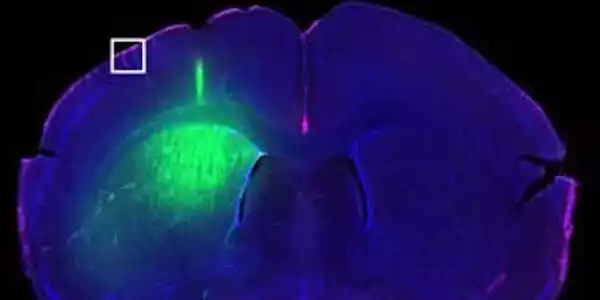
Studying mice, Kipnis, Drieu, and colleagues discovered that such macrophages regulate the motion of blood arteries that, in turn, controls the cleansing flow of fluid through the brain. When these macrophages were depleted or impaired, debris built up in the brain.
“In numerous neurodegenerative diseases, such as Alzheimer’s, stroke, Parkinson’s, and multiple sclerosis, cerebrospinal fluid flow is impaired,” Drieu said. “If we can simply boost macrophages and restore fluid flow through the brain, we may be able to slow the progression of these diseases. Who knows if it’s a dream? It could work.”
Further research revealed that parenchymal border macrophages in people with Alzheimer’s disease and mice with an Alzheimer’s-like condition are altered: the immune cells are less able to consume and dispose of waste, and they cannot regulate fluid flow efficiently.
Starting at about age 50, people start experiencing a decline in brain fluid flow as part of normal aging. The same thing happens in older mice. Kipnis, Drieu, and colleagues showed that the kind of border macrophage most important for waste clearance and fluid flow are scarce in older mice. When they treated old mice with a protein that boosts macrophage activity, the border macrophages started behaving more like those from younger mice. Further, the treatment improved fluid flow and waste clearance from the mice’s brains.
“Our findings suggest that parenchymal border macrophages could potentially be targeted pharmacologically to alleviate brain clearance deficits associated with aging and Alzheimer’s disease,” said Kipnis, who is also a professor of neurology, neuroscience, and neurosurgery. “I’m talking with colleagues about how we can replace or rejuvenate those cells in aging brains and as a treatment for Alzheimer’s. With this approach, I hope that one day we will be able to slow or delay the development of age-related brain diseases.”