Numerous lines of evidence point to a link between immunological malfunction and psychiatric diseases such as schizophrenia, autism spectrum disorders, and depression. There is strong evidence for increased circulating levels of proinflammatory cytokines prior to illness onset, and epidemiological studies have shown that exposure to a variety of infections during prenatal life and childhood is associated with an increased risk of schizophrenia and autism spectrum disorder.
Researchers at the University of Birmingham have discovered a possible relationship between inflammation and the anatomy of specific brain regions. The findings, which was published in JAMA Psychiatry, may be especially relevant for neurodevelopmental psychiatric diseases such as autism spectrum disorder and schizophrenia.
According to the researchers, the findings potentially open up a whole new target for the pharmacological treatment of these disorders, which has not changed considerably since the discovery of antipsychotic drugs in the mid-late twentieth century.
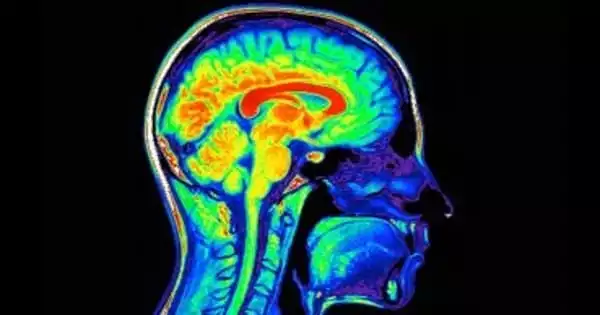
The study was conducted by a team from the University’s Institutes of Mental Health and Cancer and Genomic Sciences, with collaborators from the Universities of Cambridge, Manchester, and Bristol. It discovered that genes related with inflammation, specifically interleukin (IL) 6, are associated with a decrease in grey matter volume in parts of the brain known to be involved in neuropsychiatric diseases.
This work demonstrates that the IL-6 gene, which has been linked to systemic inflammation, impacts brain structure in areas associated with various neuropsychiatric illnesses. Understanding these connections opens up the possibility of developing new IL-6-targeting medicines.
Professor Rachel Upthegrove
The team was able to correlate genetic variations that impact levels of IL-6 and other inflammatory genes in more than 20,000 patients with changes in grey matter volume in specific parts of the brain using records from the UK Biobank, a large-scale scientific database.
They were able to demonstrate robust correlations between IL-6 and brain anatomy, especially in the temporal and frontal areas. Using the Allen Human Brain Atlas, researchers discovered that genes overexpressed in these locations are linked to disorders such as epilepsy, cognitive dysfunction, and schizophrenia.
The paper’s principal author is Professor Rachel Upthegrove of the University’s Institute for Mental Health. She stated: “This work demonstrates that the IL-6 gene, which has been linked to systemic inflammation, impacts brain structure in areas associated with various neuropsychiatric illnesses. Understanding these connections opens up the possibility of developing new IL-6-targeting medicines. This could be the first new target for serious mental diseases such as schizophrenia in well over 60 years.”

“Current medicines for these conditions operate on dopamine, a chemical messenger in the brain related with mood and attention,” said Dr. John Williams of the University’s Institute for Cancer and Genomic Sciences, a first author on the report. These medications, however, can have negative effects and are not successful in all people. There are existing medications on the market that target inflammation, as well as the possibility of screening possible novel molecules. It’s quite exciting to discover a new path for investigating the relationships between inflammation, brain anatomy, and neuropsychiatric diseases.”
Patients with mental problems have a variety of structural brain changes when compared to healthy controls, but the source of these differences is unknown. Interleukin 6 (IL-6) and its receptor IL-6R may be of special relevance since they can breach the blood-brain barrier and enhance its permeability, attracting more local inflammatory players, and may be associated with treatment resistance and poor functional results. Inflammation is linked to structural brain abnormalities that underpin neuropsychiatric illnesses via microglia and astrocytic function, resulting in aberrant synaptic pruning and an effect on gray matter volume (GMV).
The study is part of the PIMS (Psychosis Immune Mechanism Stratified Medicine Study) initiative, which was founded by the University of Birmingham to research the relationships between inflammation and psychosis. The researchers will conduct experimental trials to knock out IL-6 in the next phase of the research, as well as replicate the Biobank findings in other varied patient populations.