Utilizing another innovation created at MIT, diagnosing cellular breakdown in the lungs could become as simple as breathing in nanoparticle sensors and, afterward, taking a pee test that uncovers whether a growth is available.
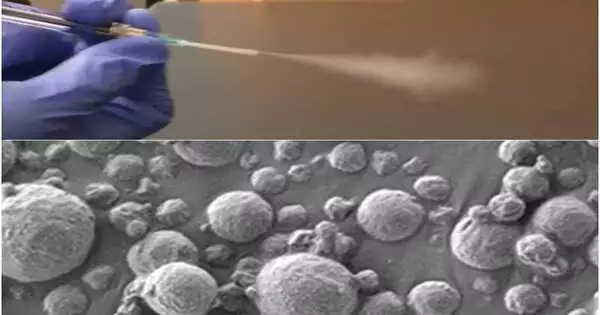
The new symptom depends on nanosensors that can be conveyed by an inhaler or a nebulizer. Assuming the sensors experience malignant growth-connected proteins in the lungs, they produce a sign that gathers in the pee, where it very well may be recognized with a straightforward paper test strip.
This approach might actually supplant or enhance the ongoing best quality level for diagnosing cellular breakdown in the lungs, low-portion processed tomography (CT). It could have a particularly huge effect in low- and middle-income nations that don’t have far-reaching accessibility to CT scanners, the scientists say.
“All over the planet, disease will turn out to be increasingly prevalent in low- and middle-income nations. The study of disease transmission of cellular breakdown in the lungs worldwide is that it’s driven by contamination and smoking, so we realize that their openness to this sort of innovation could have a major effect,” says Sangeeta Bhatia, the John and Dorothy Wilson Teacher of Wellbeing Sciences and Innovation and of Electrical Designing and Software Engineering at MIT, and an individual from MIT’s Koch Organization for Integrative Malignant Growth Exploration and the Foundation for Clinical Designing and Science.
“Cancer will grow increasingly frequent in low- and middle-income countries over the world. The epidemiology of lung cancer internationally is that it is driven by pollution and smoking, so we know that those are environments where access to this kind of technology might have a major impact.”
Sangeeta Bhatia, the John and Dorothy Wilson Professor of Health Sciences and Technology and of Electrical Engineering and Computer Science at MIT,
Bhatia is the senior creator of the paper, which shows up in Science Advances. Qian Zhong, a MIT research researcher, and Edward Tan, a previous MIT postdoc, are the lead creators of the review.
Inhalable particles
To assist with diagnosing cellular breakdown in the lungs as soon as could really be expected, the U.S. Preventive Administrations Team suggests that weighty smokers beyond 50 years old go through yearly CT checks. Nonetheless, not every person in this target bunch gets these outputs, and the high, bogus positive pace of the sweeps can prompt superfluous, obtrusive tests.
Bhatia has gone through the last ten years creating nanosensors for use in diagnosing malignant growth and different illnesses, and in this review, she and her partners investigated the chance of involving them as a more open option in contrast to CT evaluating for cellular breakdown in the lungs.
These sensors comprise polymer nanoparticles covered with a columnist, for example, a DNA scanner tag, that is separated from the molecule when the sensor experiences catalysts called proteases, which are often overactive in cancer. Those journalists, in the long run, amass in the pee and are discharged from the body.
Past renditions of the sensors, which designated other disease locales like the liver and ovaries, were intended to be given intravenously. For cellular breakdown in the lungs determination, the specialists needed to make a variant that could be breathed in, which could make it more straightforward to convey in lower asset settings.
“At the point when we fostered this innovation, our objective was to give a strategy that can recognize malignant growth with high particularity and responsiveness and furthermore bring down the edge for openness, so that ideally we can further develop the asset divergence and disparity in early identification of cellular breakdown in the lungs,” Zhong says.
That’s what they wanted to accomplish. The specialists made two plans for their particles: an answer that can be airborne and conveyed with a nebulizer and a dry powder that can be conveyed utilizing an inhaler.
When the particles arrive at the lungs, they are ingested into the tissue, where they experience any proteases that might be available. Human cells can communicate with many different proteases, and some of them are overactive in growth, where they help disease cells get away from their unique areas by slicing through proteins of the extracellular network.
These malignant proteases divide DNA scanner tags from the sensors, permitting the standardized identifications to flow in the circulation system until they are discharged in the pee.
In the prior adaptations of this innovation, the specialists utilized mass spectrometry to examine the pee test and recognize DNA scanner tags. In any case, mass spectrometry requires hardware that probably won’t be accessible in low-asset regions, so for this variant, the specialists made a sidelong stream examine, which permits the scanner tags to be recognized utilizing a paper test strip.
The specialists planned for the strip to recognize up to four different DNA-standardized identifications, each of which shows the presence of an alternate protease. No pre-treatment or handling of the pee test is required, and the outcomes can be learned about 20 minutes after the example is acquired.
“We were truly pushing this examine to be point-of-care accessible in a low-asset setting, so the thought was to not do any example handling, not do any enhancement, just to have the option to put the example right on the paper and read it out shortly,” Bhatia says.
Exact conclusion
The specialists tried their demonstrative framework in mice that are hereditarily designed to foster lung growths like those found in people. The sensors were managed 7.5 weeks after the growths began to frame, a period point that would probably correspond with stage 1 or 2 disease in people.
In their first arrangement of examinations in quite a while, the specialists estimated the degrees of 20 unique sensors intended to distinguish various proteases. Utilizing an AI calculation to dissect those outcomes, the scientists recognized a blend of only four sensors that was anticipated to give exact demonstrative outcomes. They then tried that mix in the mouse model and found that it could precisely identify beginning-phase lung growths.
For use in people, it’s conceivable that more sensors may be expected to make a precise finding; however, that could be accomplished by utilizing various paper strips, each of which distinguishes four unique DNA-standardized tags, the specialists say.
The specialists presently plan to investigate human biopsy tests to check whether the sensor boards they are utilizing would likewise attempt to identify human malignant growths. In the more drawn-out term, they desire to perform clinical preliminaries on human patients. An organization called Sunbird Bio has proactively run Stage I preliminaries on a comparative sensor created by Bhatia’s lab for use in diagnosing liver disease and a type of hepatitis known as nonalcoholic steatohepatitis (NASH).
In regions of the planet where there is restricted admittance to CT checking, this innovation could offer a sensational improvement in cellular breakdown in the lungs screening, particularly since the outcomes can be gotten during a solitary visit.
“The thought would be that you come in and afterward find a solution, regardless of whether you really want a subsequent test, and we could get patients who have early sores into the framework so they could get corrective medical procedures or lifesaving medications,” Bhatia says.
More information: Qian Zhong et al, Inhalable point-of-care urinary diagnostic platform, Science Advances (2024). DOI: 10.1126/sciadv.adj9591. www.science.org/doi/10.1126/sciadv.adj9591