A tissue-modifying chemical that can target intestinal stem cells and instruct them to generate Paneth cells, a rare but crucial cell type that can affect the gut microbiota, was found in a recent study. Paneth cells have been found to be decreased in disorders such as inflammatory bowel disease and graft-versus-host disease. Replenishing these uncommon cells may open up a new therapeutic avenue. The approach used by the team could also be used to identify compounds that could target different types of intestinal cells.
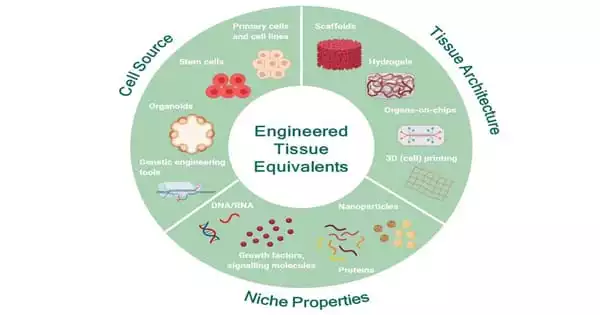
Researchers at the Brigham and Women’s Hospital and the Broad Institute have constructed specialized, tissue-like structures in the laboratory to imitate barrier tissues such as the intestines in order to uncover new therapeutic targets.
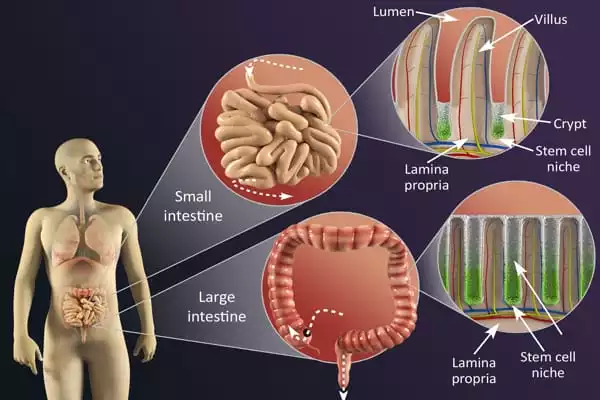
Barrier tissues are exposed to substances from the outer environment but act as a protective layer. Researchers have built more complex three-dimensional models of epithelial barrier tissues, such as the intestine, throughout the years. Intestinal organoids are the name given to these models. A tissue-modifying chemical that can target intestinal stem cells and instruct them to generate Paneth cells, a rare but crucial cell type that can affect the gut microbiota, was discovered in a new study. Paneth cells have been found to be decreased in disorders such as inflammatory bowel disease and graft-versus-host disease. Replenishing these uncommon cells may open up a new therapeutic avenue. The approach used by the team could also be used to identify compounds that could target different types of intestinal cells.
Our study gives the first method to engineering our barrier tissues like the intestine by targeting and activating stem cells in situ and inducing the formation of new essential cell types. By altering the cell makeup of the intestine, this might possibly be used to treat a wide range of disorders.
Benjamin Mead
Barrier tissue epithelia are critical in maintaining organismal homeostasis, and changes in their cellular composition have been seen in a variety of human disorders. Adult stem cells integrate several signals within the small intestine epithelium to govern regeneration and differentiation, establishing total cellularity. As a result, guiding stem cell differentiation may give a tractable way to modifying the amount or quality of specialized cells of the small intestinal epithelium, such as the secretory Paneth, goblet, and enteroendocrine populations.
“The cellular composition of barrier epithelia is required for organismal homeostasis.” Adult stem cells, in particular, create tissue cellularity inside the small intestine and may provide a mechanism to manage the amount and quality of specialized epithelial cells,” the researchers said.
“However, strategies for identifying biological targets that regulate epithelial composition and function, as well as small compounds that modulate them, are missing.” We show here that druggable biological targets and small-molecule regulators of intestinal stem cell differentiation can be identified using thousands of miniaturized organoid models of intestinal stem cell differentiation into Paneth cells and validated using longitudinal single-cell RNA-sequencing.
“Our study gives the first method to engineering our barrier tissues like the intestine by targeting and activating stem cells in situ and inducing the formation of new essential cell types,” stated Broad Institute co-lead author Benjamin Mead, PhD. “By altering the cell makeup of the intestine, this might possibly be used to treat a wide range of disorders.”
“This approach has wide ranging implications and can be used to manipulate the cellular makeup of the intestine, including cells that can enhance barrier function, produce gut hormones, or that have key roles in coordinating insulin levels as well as food digestion and absorption,” said co-corresponding author Jeff Karp, PhD, Distinguished Chair in Clinical Anesthesiology, Perioperative and Pain Medicine. “This approach also enables a completely new strategy to manipulate gut microbiota and thus offer insights into the treatment of a wide range of diseases.”
The human digestive tract’s cellular landscape is dynamic throughout life, forming in utero and changing in response to functional requirements and environmental exposures. We employ single-cell RNA sequencing and antigen receptor analyses of almost half a million cells from up to 5 anatomical regions in the developing and up to 11 unique anatomical regions in the healthy paediatric and adult human stomach to completely map cell lineages. This demonstrates the presence of BEST4 epithelial cells with unique transcriptional profiles throughout the human gastrointestinal tract.
The physiology of the gastrointestinal tract is dependent on the coordinated input of various cell lineages, the relative quantity and cell networking of which vary from embryonic development to adulthood. The intestinal tract is further complicated by the fact that it is made up of multiple anatomical sections that develop at different speeds and play varied functions in digesting, nutrition absorption, metabolism, and immunological control.