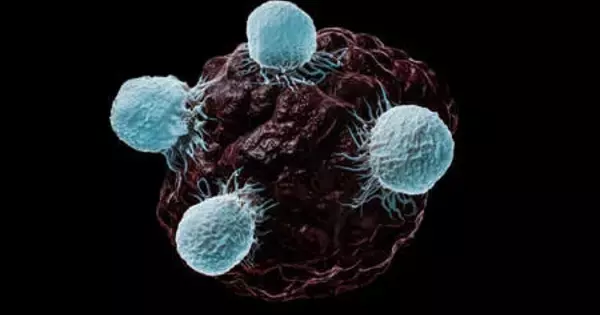
Researchers at Sanford Burnham Prebys, led by Ze’ev Ronai, Ph.D., have shown for the first time that inhibiting a key metabolic enzyme selectively kills melanoma cells and stops tumor growth. Published in Nature Cell Biology, these findings could lead to a new class of drugs to selectively treat melanoma, the most severe form of skin cancer.
“We found that melanoma is addicted to an enzyme called GCDH,” says Ronai, professor and director of the NCI-designated Cancer Center at Sanford Burnham Prebys. “If we inhibit the enzyme, it leads to changes in a key protein, called NRF2, which acquires its ability to suppress cancer. Now, our goal is to find a drug, or drugs, that limit GCDH activity, potentially new therapeutics for melanoma.”
Because tumors grow rapidly and require lots of nutrition, researchers have been investigating ways to starve cancer cells. As promising as this approach may be, the results have been less than stellar. Denied one food source, cancers invariably find others.
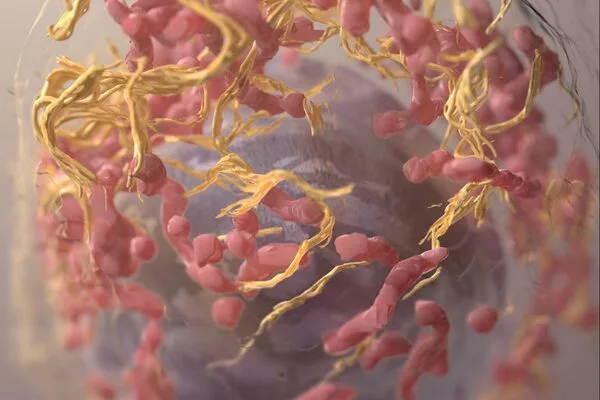
GCDH, which stands for Glutaryl-CoA Dehydrogenase, plays a significant role in metabolizing lysine and tryptophan, amino acids that are essential for human health. When the Ronai lab began interrogating how melanoma cells generate energy from lysine, they found GCDH was mission-critical.
In the study, we used genetic approaches to inhibit GCDH, which provide the proof of concept to search for small molecules inhibitors. Indeed, we are actively searching for potential drugs that could inhibit GCDH, which would be candidates for novel melanoma therapies.
Sachin Verma
“Melanoma cells ‘eat’ lysine and tryptophan to produce energy,” says Sachin Verma, Ph.D., a postdoctoral researcher in the Ronai lab and the first author of the study. “However, harnessing energy from this pathway requires cancer cells to quench toxic waste produced during this process. It’s a six-step process, and we thought the cells would need all six enzymes. But it turns out only one of these enzymes is crucial, GCDH. Melanoma cells cannot survive without the GCDH portion of the pathway.”
Further exploration showed that inhibiting GCDH in an animal model gave NRF2 cancer-suppressing properties.
“We’ve known for a long time that NRF2 can be both a driver and a suppressor of cancer,” says Ronai. “We just didn’t know how we convert NRF2 from a driver to suppressor function. Our current study identifies the answer.”
The researchers also found that inhibiting GCDH was rather selective for melanoma tumors. Similar efforts in lung, breast, and other cancers had no impact, probably because those cancers may be addicted to other enzymes.
When cells start to proliferate, their metabolic needs alter because the metabolism of those cells must support a different stage of cellular development. Because all cancer cells exhibit uncontrolled cell proliferation, cancer cells must therefore perform at a higher rate of biosynthesis. Therefore, to maintain ATP levels for optimal homeostasis, cancer cells must allocate available resources toward biosynthetic pathways.
From a therapeutic standpoint, the study reveals several possible options. Though animal models without GCDH were basically normal, they could not tolerate a high-protein diet. This is significant because some melanoma patients’ tumors are also low in GCDH. Given the enzyme’s role in processing proteins, the authors believe GCDH-poor tumors may also be vulnerable to high-protein foods, setting up a potential dietary treatment. In addition, reducing GCDH levels in tumors may be complemented with select protein diets.
GCDH inhibition shows significant therapeutic promise. Because normal cells without GCDH are mostly unaffected, GCDH inhibitors would be quite specific to melanoma cells. The Ronai lab is now working with scientists at the Conrad Prebys Center for Chemical Genomics at Sanford Burnham Prebys to identify small molecule GCDH inhibitors that could be the starting point for future melanoma treatments.
“In the study, we used genetic approaches to inhibit GCDH, which provide the proof of concept to search for small molecules inhibitors,” says Verma. “Indeed, we are actively searching for potential drugs that could inhibit GCDH, which would be candidates for novel melanoma therapies.”