A multi-institutional public review has recognized extraordinary sub-atomic highlights responsible for the turn of events and movement of metastatic breast disease. One of the key elements includes changes in the resistant framework that are expected, to some degree, to result from the methylation of the HLA-A quality; methylation is the expansion of a little compound into a DNA particle. Central cancellations, or a lack of part of the HLA-A quality, were also discovered and were fundamentally unrelated to DNA methylation tests.In this study, methylation and central erasures made less resistant cells available to go after malignant growth cells.
The findings were published in Nature Malignant growth on December 30, 2022.
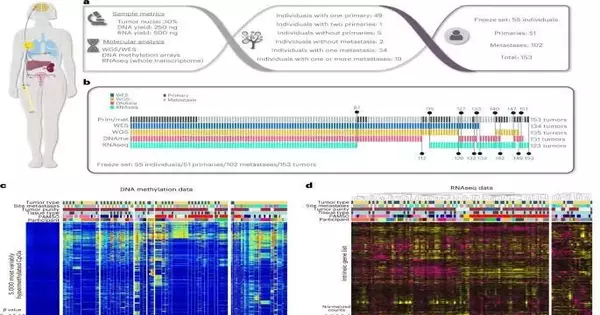
The review, driven by the AURORA US Metastasis Organization Venture, is one of the first to utilize numerous genomic stages to examine essential (unique) growths and their matched metastases; most prior examinations took a gander at essential diseases, or metastases, in separation from one another. In this new investigation of 55 ladies with metastatic bosom disease, the specialists gathered growth tissue that addressed 51 essential tumors and 102 matched metastases.
“This study included a broad joint effort among numerous foundations to propel how we might interpret bosom disease,” said Charles M. Perou, Ph.D., the May Goldman Shaw Recognized Teacher of Atomic Oncology, co-head of the UNC Lineberger Far Reaching Disease Center’s Bosom Malignant Growth Exploration Program, and the related creator of this review. “Our insight into bosom malignant growth science comes from investigations of unique cancers, yet when individuals pass on from bosom disease, it is from a metastatic infection, so our absence of comprehension of the science of metastasis impedes patient consideration.”
“Our understanding of the biology of breast cancer stems from research on primary tumors, but because metastatic illness is the cause of death from breast cancer, patient care is hampered by our ignorance of the biology of metastasis.”
Charles M. Perou, Ph.D., the May Goldman Shaw Distinguished Professor of Molecular Oncology
The specialists found that lymphocytes and B cells, which generally direct the growth-resistant reaction, were outstandingly less prevalent in metastases. They also looked at differences in metastasis destinations: liver and mind metastasis showed lower levels of safe cell reaction when compared to levels of resistant cells found in lung metastases.
“We viewed that as around 17% of metastatic growths having decreased articulation of a quality that influences cell resistance and showed a diminished capacity of safe cells to penetrate their current circumstance and ward off disease cells,” said Susana Garcia-Recio, Ph.D., an associate teacher in Perou’s lab at UNC Lineberger and co-lead creator of this review.
Notwithstanding Garcia-Recio, the paper’s other co-lead creators are Toshinori Hinoue, Ph.D., Van Andel Establishment, Terrific Rapids, MI; Gregory L. Wheeler, Ph.D., and Benjamin J. Kelly, MS, Cross Country Kids’ Medical Clinic, Columbus, Georgia; and Ana C. Garrido-Castro, MD, Dana-Farber Disease Organization, Boston.
“This finding addresses yet the main portion of the AURORA US Metastasis Organization Venture, as scientists have as of late sent off a clinical preliminary to assist with gathering more examples,” said Nancy E. Davidson, MD, Leader VP of Clinical Issues at Fred Hutchinson Cancer Research Center, Seattle, and one of the originators behind AURORA. “The results of preliminary investigations of the examples will be added to the momentum information, enabling better discovery of genomic changes to upgrade how we might interpret the illness truly.”
“We saw changes in science in around 30% of patients, including loss of safe enactment, particularly in liver and mind metastases,” said Lisa A. Carey, MD, ScM, FASCO, agent head of clinical science and the L. Richardson and Marilyn Jacobs Preyer recognized teacher in bosom malignant growth exploration at UNC Lineberger. “A significant number of these progressions happened through systems that can be switched or treated.” “As a result of this work, we are extremely excited about the potential for further developed treatment of metastatic infection, or even the prediction of metastases.”
“This pivotal review, which recognizes another objective for possibly controlling metastatic illness, exhibits the worth of wide-based cooperative examination by individuals joined by their commitment to a fundamental mission,” said Larry Norton, MD, establishing logical head of the Bosom Malignant Growth Exploration Establishment.
“We owe our patients an enormous round of gratitude for assisting us with propelling these exploration endeavors and for any commitments they make from now on,” said Perou. “We are presently mirroring a ton of these hereditary discoveries in our mouse models, where we are trying new medicines and gaining genuine headway, which we expect will pay off for patients sooner rather than later.”
More information: Susana Garcia-Recio et al, Multiomics in primary and metastatic breast tumors from the AURORA US network finds microenvironment and epigenetic drivers of metastasis, Nature Cancer (2022). DOI: 10.1038/s43018-022-00491-x