Electronic nanomembranes that are flexible have the potential to revolutionize organ-on-chip technologies and eliminate the need for animal testing in medical research.
UNSW Sydney engineers have discovered a method for fabricating flexible electronic systems on extremely thin skin-like materials.
By making organ-on-chip technology more effective, the development makes it possible for complete stretchable 3D structures to function like semiconductors. This could significantly reduce the need for animal testing.
In the future, the technology might also be put to use in wearable health monitoring systems or biomedical applications that can be implanted, like a system to tell people with epilepsy when they are about to have a seizure.
“We use a wide bandgap material, which does not absorb visible light like traditional semiconductor materials.” That means scientists may examine the organ-on-chip under a microscope, which would not be possible otherwise.”
Scientia Lecturer Dr. Thanh Nho Do, a chief investigator on the project,
The research team, led by UNSW School of Mechanical and Manufacturing Engineering’s Dr. Hoang-Phuong Phan, has published their findings in the journal Advanced Functional Materials.
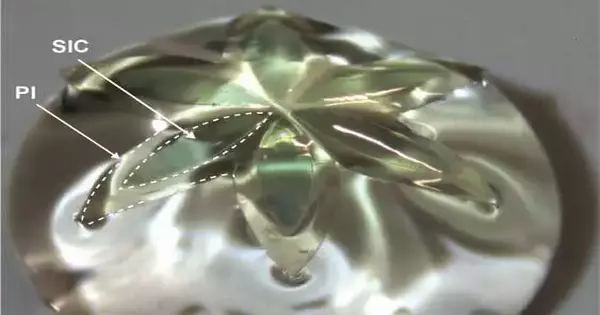
In their new method, wide-bandgap semiconductors like silicon carbide and gallium nitride are printed onto very thin and flexible nanomembranes on a polymer substrate using lithography, a method that uses light to print tiny patterns.
Organ-on-a-chip technology
These semiconductor membranes can be stretched and twisted into any three-dimensional shape and still provide sensing, recording, and stimulation functions.
They could play a significant role in the cutting-edge technology known as organ-on-chip, which creates miniature versions of human organs on tiny chips.
These chips imitate the capabilities and designs of organs, permitting researchers to concentrate on their way of behaving and test the impacts of medications or illnesses in a more precise and proficient way.
Additionally, since organ-on-chip technology enables researchers to replicate the complexity of human organs in a laboratory setting, it has the potential to eliminate the need for a wide range of tests and experiments involving animals.
Dr. Phan asserts, “For legal, ethical, and moral reasons, many people are keen to move toward medical testing on replicated versions of human cells rather than live animals.”
“You can develop 3D cell organs that emulate the organs in a genuine body, but we likewise need to foster 3D terminals to assist with working with that organ-on-chip process.”
“Our method makes it possible to create an electronic system on a membrane that can be stretched into any three-dimensional shape around the organ-on-chip.”
The work is the highlight of the cross-institutional, interdisciplinary collaboration between UNSW, Griffith University, the University of Queensland, and QUT, as well as their international partners, Kyung Hee University, the University of Southern California, and Northwestern University.
“We use wide bandgap material, which unlike traditional semiconductor materials does not absorb visible light,” said UNSW Scientia Lecturer Dr. Thanh Nho Do, a chief investigator on the project. As a result, researchers will be able to view the organ-on-chip through a microscope whenever they want to, which would not be possible otherwise.
“The electronic framework on the layer likewise permits a ton of information to be gathered while checking how the counterfeit organ is responding to various things while being tried.”
The researchers anticipate that within three to five years, a commercial product could be produced for this application. However, they intend to carry out additional research to further enhance the device and incorporate additional components like wireless communication.
According to Dr. Phan, the new method has the intriguing potential to significantly enhance the quality of monitoring, diagnosis, and treatment when applied to wearable health monitoring systems.
A wearable sleeve that helps detect and signal alerts regarding the levels of UV radiation a person is exposed to throughout the day could have one such function. This could ultimately help reduce the number of cases of skin cancer.
According to Dr. Phan, “the wide bandgap material is important for that application because traditional silicon semiconductors have a narrow bandgap and do not absorb UV light.”
Neuron signals
The UNSW group likewise proposes that their new material might be grown further to make implantable biomedical gadgets where the electrical framework can screen and impact neuron signals continuously.
Even though such a device probably won’t be available for at least ten years, the researchers are already planning additional tests to see if they can help people with epilepsy, a neurological disorder in which seizures can be caused by sudden and uncontrolled bursts of electrical activity in the brain.
According to Dr. Phan, “when a seizure is just about to happen for people with epilepsy, the brain will send out unusual signals that are the trigger.”
“It may also be used to apply electrical stimulation to bypass the seizure if we can create an implantable electronic device that can detect those abnormal patterns.”
One of the key issues that should be addressed concerning implantable gadgets is the way to power such an electronic framework.
As a result, researchers at UNSW are also working on the creation of a magnetic resonance coupling system that could be incorporated into the wide-bandgap 3D electronic membranes in order to wirelessly transmit power through the body using an external antenna.
More information: Thanh‐An Truong et al, Engineering Route for Stretchable, 3D Microarchitectures of Wide Bandgap Semiconductors for Biomedical Applications, Advanced Functional Materials (2023). DOI: 10.1002/adfm.202211781