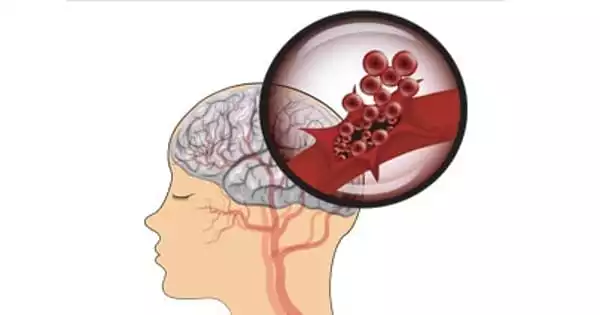
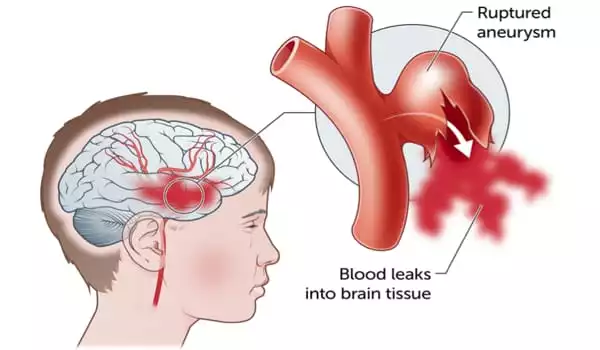
A newborn brain bleed is a rather common consequence of childbirth. This happens when blood vessels rupture and hemorrhage into brain tissue. It is also referred to as intracranial hemorrhage (ICH) or intraventricular hemorrhage (IVH) (IVH). The intensity and location of the brain hemorrhage influence the severity of the injury. Researchers have discovered a novel method for identifying babies and fetuses who are at high risk of experiencing brain bleeds, paving the possibility for improved early management.
WEHI (Walter and Eliza Hall Institute) researchers have discovered a new method for identifying babies and foetuses at high risk of experiencing brain bleeds, paving the path for better early management.
Brain bleeding in pregnant fetuses and neonates can result in stroke and lasting neurological disorders such as cerebral palsy. A brain bleed can occur for a variety of reasons. Premature babies are much more susceptible to have this ailment due to their immature circulation. However, a brain bleed can occur in term delivery babies.
We need to see how, or even if, platelets and brain blood arteries collaborate to establish resistance to brain bleeds. Our next great task is to figure out if brain bleeds are caused by a breakdown in communication between platelets and blood vessels, or if they are driven by environmental variables.
Dr. Samir Taoudi
While platelet transfusions can sometimes be used to heal brain bleeds, the intrusive procedures are risky, and it was unclear which newborns would benefit the most.
At a glance
- Novel research identifies a new method for identifying prenatal and newborn newborns at risk of brain bleeds.
- Preclinical investigations reveal that brain bleeds develop when platelet levels in foetuses and neonates fall to 10% or below.
- The new threshold might be used to select which newborns should be treated, revolutionizing platelet transfusion practices and minimizing wasteful treatments.
Dr. Alison Farley and Dr. Samir Taoudi of WEHI are examining how platelet levels, small blood cells best known for facilitating blood clots, affect brain bleeds in order to better understand when platelet transfusion should be used.
A new study of preclinical models discovered that brain bleeds invariably occurred when platelet levels in neonates and foetuses decreased to 10% or lower. The research also suggests that babies may develop protection against brain bleeds two weeks after birth, with bleeding no longer triggered by very low platelet levels after this age.
The study, which was published in Blood, lays the way for a better understanding of which babies should receive a platelet transfusion and where the platelet threshold should be placed to avoid unnecessary transfusions.
Platelet counts
Low platelet levels, often known as thrombocytopenia, can cause excessive bleeding and are prevalent in premature infants. Researchers were able to discern three levels of platelet counts that determined brain bleed risk by analyzing varying degrees of thrombocytopenia in pre-clinical mice.
They discovered that brain bleeds in pregnant or newborn newborns were assured if their platelet count dropped to 10% or lower. While a moderate platelet count of 10-40% could potentially cause a brain hemorrhage, newborns with more than 40% platelets were not at risk of developing the illness at all.
“At the moment, platelet transfusions are provided to babies in that intermediate range who may not even develop brain bleeds,” Dr Farley explained.
“It is crucial to determine the platelet levels that will always result in brain bleeds and those that will not. Our findings could aid in determining which newborns can safely receive platelet transfusions after birth, and where the threshold could be decreased to minimize unneeded and hazardous transfusions. If platelet loss starts within days of birth, there may be a window for effective intervention to avert catastrophic brain bleeds and stroke in neonates.”
Building resistance
Dr. Samir Taoudi stated that the next stage would be to investigate why protection against brain bleeds occurs two weeks after birth, as well as which proteins and genes are involved.
“We need to see how, or even if, platelets and brain blood arteries collaborate to establish resistance to brain bleeds,” said Dr Taoudi. “Our next great task is to figure out if brain bleeds are caused by a breakdown in communication between platelets and blood vessels, or if they are driven by environmental variables.”