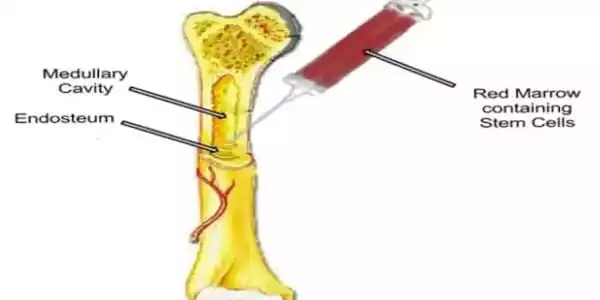
Bone marrow transplantation (BMT) is a specialized treatment for people suffering from cancer or other disorders. A bone marrow transplant entails extracting cells that are ordinarily found in bone marrow (stem cells), purifying those cells, and returning them to either the donor (patient) or another person. The purpose of BMT is to transfuse healthy bone marrow cells into a person after his or her own unhealthy bone marrow has been treated to destroy the abnormal cells.
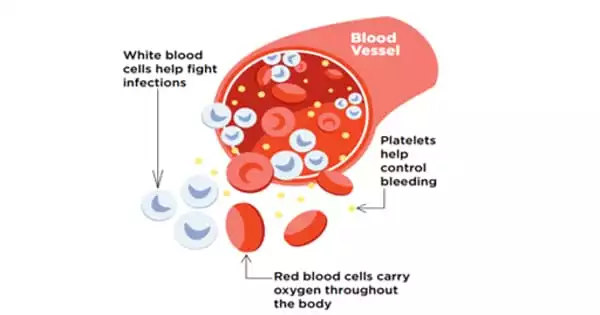
After being implanted into patients with blood cell-related disorders, hematopoietic stem cells can develop and produce healthy blood cells. The unique signature of genes expressed by these cells has recently been revealed by researchers. Scientists may be able to increase these cells or convert other types of cells into cells that can repopulate the blood system as a result of the discovery, which could have substantial clinical implications. In the future, this research could help with the treatment of a variety of ailments or allow for the generation of an infinite supply of these uncommon cells from more common cell types.
Hematopoietic stem cells (HSCs) have the ability to self-renew and specialize into all mature blood cell types, making them viable therapies for a wide range of disorders. However, the mechanisms underlying engraftment (when cells begin to proliferate and produce healthy blood cells after being transplanted into a patient) remain unknown.
Overall, our research has produced a thorough blueprint of the most potent blood stem cells, which will lead to a deeper understanding of why these cells have such exceptional regenerative capacity. These discoveries will enable us to develop safer and more effective medicines for patients suffering from blood diseases.
Kim Vanuytsel
A recent study headed by researchers at Massachusetts General Hospital (MGH) and Boston University School of Medicine identified the distinct signature of genes expressed by HSCs capable of undergoing this procedure. The results, which were published in Nature Communications, could allow scientists to multiply these cells outside of the body or transform other types of stem cells into cells that can repopulate the blood system.
HSCs are found in the bone marrow and circulation in adults, but they are more abundant in the liver before birth, where they grow, or proliferate, into new HSCs at a rapid rate. Furthermore, animal studies have demonstrated that HSCs from the fetal liver are more capable of engraftment than HSCs from bone marrow.
To learn more about what gives fetal liver HSCs their superior proliferation and engraftment abilities, researchers studied the gene expression patterns that are specific to these very potent stem cells. This assessment was complemented with a number of experimental methods to describe the protein expression and functionality of those same cells.
“This in-depth analysis revealed that these stem cells express a protein on their surface called CD201 that correlates very closely with this engraftment potential and can be used to isolate functional stem cells away from other cell types,” says co-senior author Alejandro B. Balazs, Ph.D., a principal investigator at the Ragon Institute of MGH, MIT, and Harvard. “This will help us improve the process of bone marrow and stem cell transplantation by allowing us to purify these cells.”
The improved understanding of the genes involved will also allow scientists to grow HSCs with high engraftment potential in the lab and alter them to combat blood cell-related disorders including sickle cell anemia, HIV, and certain types of cancer more effectively.
“Overall, our research has produced a thorough blueprint of the most potent blood stem cells, which will lead to a deeper understanding of why these cells have such exceptional regenerative capacity. These discoveries will enable us to develop safer and more effective medicines for patients suffering from blood diseases” Kim Vanuytsel, Ph.D., a research assistant professor of medicine at Boston University School of Medicine, is the study’s lead author.
Co-senior author George J. Murphy, Ph.D., an associate professor of medicine at Boston University School of Medicine and co-founder of the BU and BMC Center for Regenerative Medicine (CReM), adds that the team’s openly shared resource, which is available in an interactive format at https://engraftable-hsc.cells.ucsc.edu, will allow for new biological insights into engraftment potential and stimulate a wide range of future studies.
“This significant work would not have been possible without the powerful, collaborative collaborations that occurred across Boston area institutions. This study is also an excellent example of ‘open-source biology’ at action, in which freely shared information and insights can be used by everybody for future discoveries” he claims.
The purpose of a bone marrow transplant is to cure numerous illnesses and kinds of cancer. A bone marrow transplant may be required when the doses of chemotherapy or radiation required to cure a malignancy are so high that the treatment permanently damages or destroys a person’s bone marrow stem cells. Bone marrow transplants may also be required if the bone marrow has been damaged by a disease.