In the most recent step toward battling neovascular age-related macular degeneration (nAMD), a group led by Teacher Nathan Gianneschi from the Global Organization for Nanotechnology at Northwestern College has disclosed an original methodology that could change patients’ lives around the world.
Their examination, distributed in Science Advances, presents thrombospondin-1 mimetic protein-like polymers (TSP1 PLPs) as an expected major advantage in the battle against this driving reason for visual deficiency.
Grasping the test: Neovascular age-related macular degeneration (nAMD)
Prior to diving into the development of Gianneschi and his group, grasping the gravity of nAMD was significant. This condition is the essential driver of visual impairment in developed countries, leaving millions wrestling with decaying visual perception and lessened personal satisfaction. While compelling for the vast majority, current medicines miss the mark for a critical segment of patients, highlighting the dire requirement for elective treatments.
“A long time ago, we were made mindful of the way that a few patients don’t answer current therapeutics in discussions with Profs. Jeremy Lavine and Greg Schwartz in Ophthalmology at Northwestern Feinberg Institute of Medication. We shaped a multidisciplinary group to handle the issue by impersonating a protein with our polymer innovation, guessed to assume a vital part in the fundamental pathway,” said Gianneschi.
“Several years ago, during discussions with Professors Jeremy Lavine and Greg Schwartz in the Department of Ophthalmology at Northwestern’s Feinberg School of Medicine, we learned that certain patients do not react to the treatments that are currently available. To address this issue, our multidisciplinary team used our polymer technology to mimic a protein that is thought to be essential to the required pathway.”
Professor Nathan Gianneschi from the International Institute for Nanotechnology
Enter TSP1 proteomimetic polymers: A beam of trust
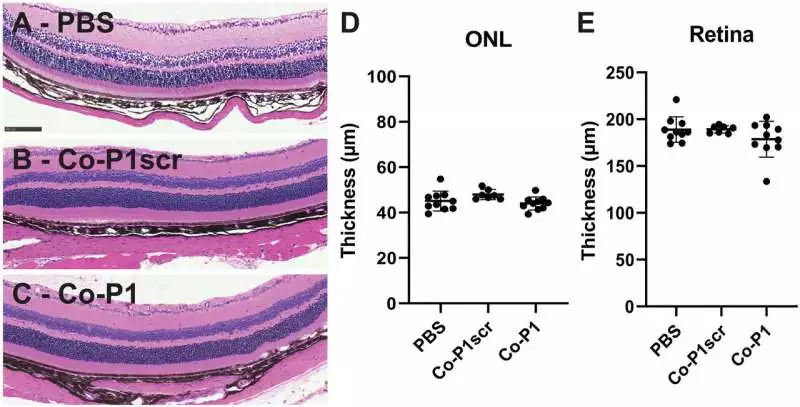
Gianneschi and his partners have imagined proteomimetic polymers, manufactured compounds designed to impersonate the way normal proteins behave, as a likely arrangement. Their review is based on thrombospondin-1 (TSP1), a protein known for restraining angiogenesis and shaping fresh blood vessels. In nAMD, strange angiogenesis adds to vision misfortune. By planning TSP1 PLPs, the specialists expected to outfit the force of this regular enemy of angiogenic specialists in a momentous way.
Their nano-size scale separates TSP1 PLPs, making them extraordinarily productive at focusing on unambiguous cell processes, similar to a neutralizer but synthetic. By restricting CD36, a vital participant in the angiogenesis guideline, these proteomimetic polymers obstruct the strange vein development normal for nAMD. Their humble size empowers them to explore the mind-boggling visual climate.
“Our polymers act to draw in the vital receptor in a multivalent way. This is like the way that we get things with our whole hand rather than with one finger. It implies we can hang on close. The PLPs do this, yet at cell receptors at the rear of the eye,” said Gianneschi.
Besides, these nanowonders show exceptional selectivity, dependability, and life span inside the eye, guaranteeing a sustained restorative impact. Their nano-scale aspects upgrade their organic collaborations and make ready for insignificantly obtrusive conveyance techniques, promising better understanding and results.
Gianneschi and his cooperation feature the extraordinary capability of nanotechnology in medication. By utilizing the standards of nanoscience, scientists are unwinding the intricacies of organic frameworks as well as designing arrangements that were once consigned to the domain of sci-fi. Gianneschi’s TSP1 PLPs address a demonstration of the noteworthy headway made in the field, offering a brief look into a future where nanoscale developments rethink the scene of clinical medicines.
More information: Wonmin Choi et al. Thrombospondin-1 proteomimetic polymers exhibit anti-angiogenic activity in a neovascular age-related macular degeneration mouse model, Science Advances (2023). DOI: 10.1126/sciadv.adi8534