Rapid diagnostic tests, used as part of the “test-treat-track” strategy in Ethiopia, the continent’s second-most populous nation, have been a key instrument in the fight against malaria in Africa.
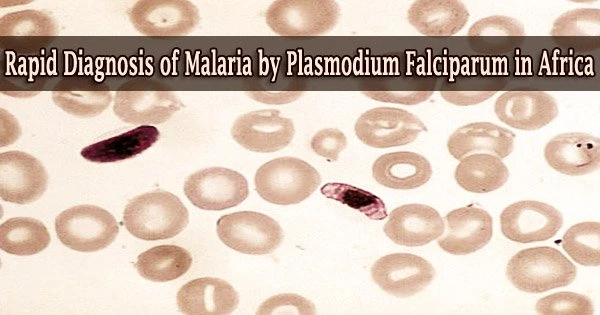
The parasite Plasmodium falciparum, the most prevalent cause of malaria cases and deaths, was overlooked by these tests, according to researchers who studied blood samples from more than 12,000 people in Ethiopia.
The study, which was published in Nature Microbiology, demonstrated that the parasite’s two genetic alterations enable it to avoid detection.
“This is a serious problem for malaria control efforts and a reminder that pathogens are very capable of adapting to survive,” said senior author Jonathan B. Parr, MD, assistant professor in the division of infectious diseases at the UNC School of Medicine. “Surveillance across the Horn of Africa and alternative malaria diagnostic approaches in affected regions are urgently needed.”
Co-corresponding authors are Sindew M. Feleke, MSc, at the Ethiopian Public Health Institute, Jane Cunningham, MD, at the WHO, and Dr. Parr.
The Ethiopian Public Health Institute and the World Health Organization (WHO) collaborated on this study endeavor.
The WHO recommends that all malaria endemic countries start and maintain surveillance for pfhrp2/3 deletions and respond appropriately when they are confirmed, in order to prevent unnecessary morbidity and deaths and to safeguard inroads that have been made towards malaria elimination, particularly in sub-Saharan Africa.
Jane Cunningham
Using RDTs, PCR diagnostics, an ultrasensitive immunoassay for antigen detection, and next-generation sequencing, the research team enrolled 12,572 participants along Ethiopia’s border with Eritrea, Sudan, and South Sudan. They discovered that P. falciparum lacking the genes histidine-rich protein 2 (pfhrp2) and histidine-rich protein 3 (pfhrp3) escape detection by the RDTs and appear to have spread quickly.
In collaboration with Brown University’s Jeffrey A. Bailey, MD, PhD, and Ozkan Aydemir, PhD, the researchers applied a molecular sequencing approach to pinpoint the particular deletion patterns of these genetic mutations.
“Our method allowed us to study the rich genomic information surrounding these genes in fine detail and at scale, facilitating the identification of evolutionary origins of these deletions,” Aydemir said.
“Our work indicates that prhrp3 deletions have arisen independently multiple times over the course of years,” said Parr, who is a member of the UNC Institute for Global Health and Infectious Diseases.
“We also found signs that RDT-based testing and treatment are driving a recent rise in pfhrp2 deletion mutation prevalence, allowing parasites to escape detection.”
In the Nature Microbiology paper, the authors ask, “What other advantages might pfhrp2/3-deleted parasites have over those with intact genes? Our limited understanding of the biology of these deletions makes this question hard to answer.”
But the authors posit several lines of inquiry in the paper, though one thing is certain.
Parr said, “We found clear evidence that parasites have recently evolved to escape detection by malaria rapid diagnostic tests along Ethiopia’s borders with Sudan and Eritrea. False-negative results were common in multiple sites and will lead to misdiagnosis and malaria deaths without intervention.”
“The results of this joint research effort have prompted us to change our diagnostic testing policies from HRP2/3-detecting RDTs to non-HRP2/3 targeted RDTs in the most affected regions of Ethiopia,” Feleke said.
Additionally, this study, along with a number of other unpublished investigations, led the WHO to issue a statement of concern.
Cunningham, said, “The WHO recommends that all malaria endemic countries start and maintain surveillance for pfhrp2/3 deletions and respond appropriately when they are confirmed, in order to prevent unnecessary morbidity and deaths and to safeguard inroads that have been made towards malaria elimination, particularly in sub-Saharan Africa.”