Radiation, which is used to treat half of all disease patients, can be estimated during therapy, which is made interesting by the University of Michigan’s exact 3D imaging.
Clinical experts can plan the radiation portion inside the body by catching and enhancing the small sound waves produced when X-rays heat tissues in the body, providing them with new information to gradually direct therapies.It’s a first-of-its-kind perspective on a cooperation specialist who has recently been unable to “see.”
“When you begin conveying radiation, the body is basically a black box,” said Xueding Wang, the Jonathan Rubin University Teacher of Biomedical Designing, Teacher of Radiology, and Related Creator of the Concentrate in Nature Biotechnology. He likewise leads U-M’s optical imaging research facility.
“In the future, we may be able to use imaging data to adjust for uncertainties caused by placement, organ motion, and anatomical variation during radiation therapy.”
Wei Zhang, a research investigator in biomedical engineering
“We don’t know precisely where the X-beams are hitting inside the body, and we don’t have the foggiest idea how much radiation we’re conveying to the objective.” Also, each body is unique, so making expectations for the two viewpoints is interesting.
Radiation is utilized in therapy for countless disease patients every year, assaulting a region of the body with high-energy waves and particles, generally X-beams. Radiation can either kill disease cells completely or harm them so that they cannot spread.
These advantages are sabotaged by an absence of accuracy, as radiation therapy frequently kills and harms cells in the region encompassing a tumor. It can likewise raise the risk of growing new malignant growths.
With continuous 3D imaging, specialists can all the more precisely direct the radiation toward malignant cells and cut off the openness of neighboring tissues. That’s what they have to do; they essentially have to “tune in.”
At the point when X-beams are consumed by tissues in the body, they are transformed into nuclear power. That warming makes the tissue grow quickly, and that extension makes a sound wave.
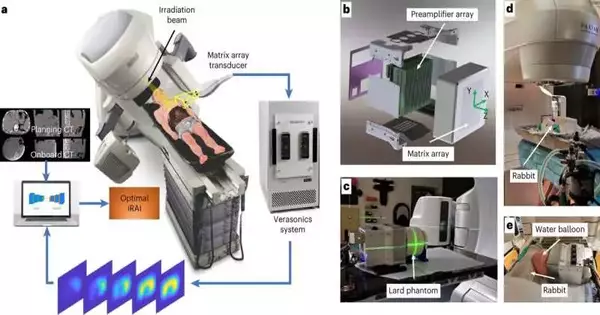
By common ultrasound innovation, the acoustic wave is frail and generally imperceptible.U-M’s new ionizing radiation acoustic imaging framework recognizes the wave with a variety of ultrasonic transducers situated on the patient’s side. The sign is intensified and then moved into an ultrasound gadget for picture reproduction.
With the pictures close by, an oncology center can change the level or direction of radiation during the interaction to guarantee more secure and successful therapies.
“Later on, we could utilize the imaging data to make up for vulnerabilities that emerge from situating, organ movement, and physical variety during radiation treatment,” said Wei Zhang, an exploration specialist in biomedical designing and the concentrate’s most memorable creator. “That would allow us to precisely convey the portion of the disease to cancer.”
One more advantage of U-M’s innovation is that it tends to be easily added to current radiation treatment gear without definitely changing the cycles that clinicians are used to.
“In later applications, this innovation can be utilized to customize and adjust every radiation therapy to guarantee typical tissues are kept to a protected portion and that the growth gets the portion planned,” said Kyle Cuneo, academic administrator of radiation oncology at Michigan Medicine. “This innovation would be particularly valuable in circumstances where the objective is nearby radiation-touchy organs like the little gut or stomach.”
The exploration group is driven by U-M, including Wang, Cuneo, and Issam El Naqa, assistant lecturer of radiation oncology at the U-M Clinical School. The group works with accomplices at the Moffitt Malignant Growth Place.
More information: Wei Zhang et al, Real-time, volumetric imaging of radiation dose delivery deep into the liver during cancer treatment, Nature Biotechnology (2023). DOI: 10.1038/s41587-022-01593-8
Journal information: Nature Biotechnology