A statistical model has been developed by researchers at the UT Southwestern Medical Center to establish standards for typical, high, or low rates of bleeding following pediatric tonsillectomies. The results, which were published in JAMA Otolaryngology-Head and Neck Surgery, may aid medical professionals in enhancing outcomes for the third-most frequent pediatric surgery in the U.S.
“This model is a practical tool for quality and safety initiatives involving tonsillectomies. Doctor Romaine Johnson, the first author, said that now that a model has been validated, doctors can compare their bleeding rates to it. as well as the Director of Quality and Safety for the Department of Otolaryngology-Head and Neck Surgery at UTSW.
The American Academy of Otolaryngology-Head and Neck Surgery Foundation updated its recommendations for pediatric tonsillectomies in 2019 and suggested that surgeons self-monitor their patients’ bleeding rates following these operations. Dr. Ron Mitchell The lead author on both the current study and those guidelines was UTSW Professor of Otolaryngology-Head and Neck Surgery and Chief of Pediatric Otolaryngology.
“This model is a good tool to incorporate in quality and safety programs involving tonsillectomies. Doctors now have a verified model against which to compare their bleeding rates.”
Romaine Johnson, M.D., Professor of Otolaryngology-Head and Neck Surgery at UTSW.
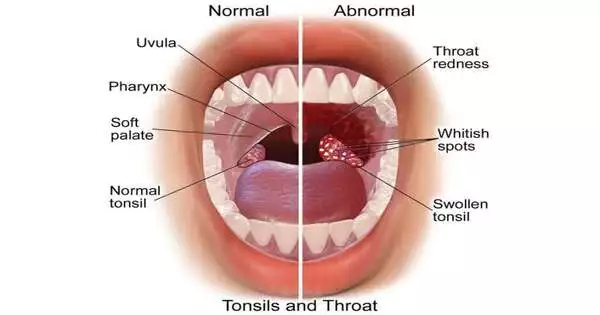
Dr. Dot Johnson noted that although complications following tonsillectomies are uncommon, excessive bleeding is one of them and is frequently blamed for the very few deaths related to this procedure. According to him, the updated recommendations were a big step toward increasing the safety of tonsillectomy procedures, but doctors still had a tough time actually using them. Doctors were not informed of the normal, high, or low bleeding rates for their institutions or themselves by any standards.
Dr. Dot Johnson and his team used the Pediatric Health Information System database, which contains de-identified patient information covering inpatient stays, outpatient surgeries, emergency department visits, and observation unit patient data from more than 49 nonprofit children’s hospitals in the U., to create probability standards. S.
The patients’ ER visits or readmissions for bleeding following tonsillectomies—a sign that their post-procedure bleeding was deemed excessive—were of particular interest to the researchers. Along with medical histories, researchers gathered demographic information about these patients.
The team discovered that the median probability rate for bleeding among all patients was 1 point 97 percent after stratifying bleeding rates for these institutions into percentiles. The rates ranged from just over one percent at their lowest point to six points and four percent at their highest point, which is in the 99th percentile. The following factors were linked to higher rates of post-tonsillectomy bleeding: adolescent age (older than 12), hispanic ethnicity, living in a relatively high-wealth ZIP code, and obesity.
Dr. Johnson emphasized that the study did not take surgical technique or the variety of tools used in tonsillectomies into account. According to him, different surgical training could have an impact on outcomes. This is an unpredictable variable. However, Dr. Johnson emphasized that there are many other factors, such as a patient’s age or other comorbidities, that influence risk and may not be to blame for higher bleeding rates.
Dr. Dot Johnson stated that “this model provides a useful starting point to help surgeons look critically at their own bleeding rates and help them understand why this complication might occur.”
More information: Romaine F. Johnson et al, Estimated Probability Distribution of Bleeding After Pediatric Tonsillectomy, JAMA Otolaryngology–Head & Neck Surgery (2023). DOI: 10.1001/jamaoto.2023.0268