Studying the biological underpinnings of psychiatric disorders is extremely challenging, in part because it is challenging to obtain brain cells from living individuals for laboratory research. Now, researchers from the University of Utah Health have created a workaround for that.
The scientists used blood cells donated by a child with pediatric bipolar disorder and by several family members to create three-dimensional structures known as “organoids.” The method discovered important molecular alterations connected to the psychiatric condition.
The findings, which were published in the journal Molecular Psychiatry, imply that structural changes in the brain seen in children and young adults with pediatric bipolar disorder may be caused by a gene that aids in cellular signaling being dysfunctional. The findings also show that organoids created in a lab can shed light on the origins of psychiatric disorders.
“To research the altered cellular and molecular pathways in pediatric bipolar disorder, new, creative models must undoubtedly be developed.”
Alex Shcheglovitov, Ph.D., assistant professor of neurobiology at University of Utah.
“There is no way to search for therapies in preclinical studies without using animal models. The task is extremely difficult, claims Dr. Alex Shcheglovitov, senior author of the study and assistant professor of neurobiology at the University of Utah. The first author of the paper is graduate student Guang Yang. To study the disrupted cellular and molecular mechanisms in pediatric bipolar disorder, there is unquestionably a need to create new, creative models.”.
The bipolar brain’s alterations.
Extreme mood swings, varying between mania and depression, are a symptom of bipolar disorder, a mental health condition. A strong genetic component may be present if the disease first manifests in childhood. A novel, multidisciplinary approach was necessary to study such a complex disorder, according to Shcheglovitov and colleagues.
Melissa Lopez-Larson, MDot Brain imaging has been performed on children with pediatric bipolar disorder and their unaffected family members by a psychiatrist and co-author of the paper to examine how the illness alters the connections between brain regions. Functional MRI, also known as fMRI, is a type of imaging that can reveal changes in the brain’s resting activity in people with bipolar disorder, though it is unknown what causes these changes.
By combining imaging data with a thorough molecular analysis of patient cells, Lopez-Larson and the neurobiologists Shcheglovitov and Yang, as well as radiologists, geneticists, and psychiatrists at the University of Utah Health and the Huntsman Mental Health Institute, were able to learn more.
Yang’s initial treatment consisted of using blood cells from a 9-year-old boy who had bipolar disorder, his parents, and a sibling who was unaffected. Yang induced the cells to develop into stem cells by cultivating them under the proper circumstances, from which he then grew neurons. An approach recently developed by the Shcheglovitov group was then used to transform the cells into structured clusters, known as organoids. Organoids allow scientists to study communication between neurons in a way that is similar to interactions that take place in the living brain by simulating the early stages of human brain development.
According to Shcheglovitov, “what these organoids allow us to do is model certain developmental stages associated with certain brain regions.”. “In our case, the organoids are more similar to the frontal region of a developing human brain.”.

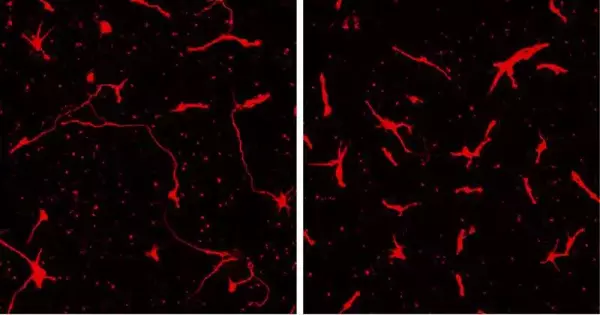
Human cells are cultured in the lab to form organoids that resemble seeds with brains. They’re identifying variations that, in some cases, may be responsible for pediatric bipolar disorder. Credit: Trevor Tanner and Nika Romero.
Looking for a reason.
Yang conducted tests to see how the cells from the child with bipolar disorder differed from those of his family members in order to identify the underlying causes of the disorder. Yang found a mutation in the PLXNB1 gene, which had previously been linked to psychiatric illness in the patient. Additionally, he discovered that cells had a different appearance: the so-called “neurites” of neurons were shorter. Normal connections between these protracted tendrils and nearby cells are significant.
Neurites in the patient’s cells grew to their normal size when normal PLXNB1 was added, proving that the changes in neurite growth were caused by the mutation in PLXNB1. Shcheglovitov declares that this is incredibly exciting. “This suggests that, possibly, using gene-based therapy or another medication that targets the PLXNB1 pathway could be therapeutically relevant for patients with pediatric bipolar disorder.”.
Researchers will need to conduct larger studies to ascertain whether other people with this disorder share these same differences before the findings can result in new therapies. Lopez-Larson claims that the strength of this study was the integration of various technologies to produce a thorough picture of what is occurring in the brain.
The fMRI revealed abnormal brain connections, at least in this particular child. And we also discovered that the genetic component supported that,” says Lopez-Larson. We had access to a variety of cutting-edge technologies that revealed the same thing in various ways.
More information: Guang Yang et al, Neurite outgrowth deficits caused by rare PLXNB1 mutation in pediatric bipolar disorder, Molecular Psychiatry (2023). DOI: 10.1038/s41380-023-02035-w