Head and neck cancers continue to be among the most deadly types of cancer despite advancements in their genomic characteristics and the availability of few targeted therapies. The presence of multiple subpopulations of cells with distinct genomic and molecular alterations, with some cells naturally more resistant to certain treatments, presents a significant obstacle to the development of effective treatments.
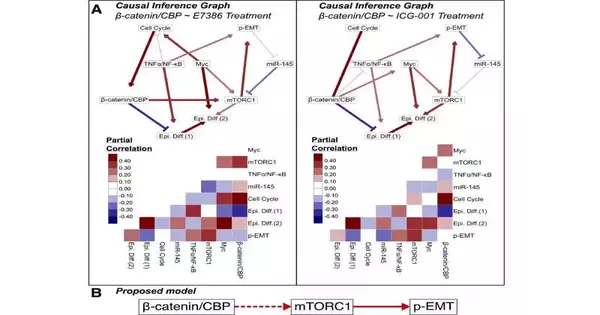
Activation of mTORC1 by b-catenin/CBP as an upstream driver of the malignancy-associated partial epithelial-mesenchymal transition (p-EMT) phenotype was discovered in a new study by researchers at Boston University Chobanian and Avedisian School of Medicine. The researchers used advanced bioinformatics and machine learning approaches to analyze large multi-omics datasets of head and neck cancer.
EMT is a biological process that is necessary for the development of an embryo, the repair of damaged tissue, and a variety of diseases, including cancer. EMT refers to the transformation of epithelial cells into mesenchymal cells, which are more migratory and invasive than epithelial cells and are typically found in the outer layers of organs.
“This is of particular interest because p-EMT is a cellular process that is an early predictor of nodal metastasis, in which epithelial cells manifest characteristics of mesenchymal cells but do not fully undergo the complete transition, and because both mTORC1 and b-cateninare important cancer hallmarks,”
Stefano Monti, Ph.D., associate professor of medicine at the School of Medicine.
Co-corresponding author Stefano Monti, Ph.D., associate professor of medicine at the School of Medicine, explained, “This is of particular interest because both mTORC1 and b-catenin are important hallmarks of cancer, and p-EMT is a cellular process that is an early predictor of nodal metastasis, in which epithelial cells manifest characteristics of mesenchymal cells but do not fully undergo the complete transition.”
“The study’s ultimate objective was to identify candidate vulnerabilities that could be targeted therapeutically,” the researchers stated. “The study aimed to better characterize oral tumor heterogeneity, including the aggressive cell subpopulations more likely to drive the early steps in cancer progression and invasiveness. “Understanding and tending to the different qualities inside growths can assist with upgrading helpful methodologies, further developing treatment results, and eventually improving patient endurance rates,” said Monti.
New computational techniques were used in this multidisciplinary collaborative study to analyze single cell data from primary oral cancer lesions. The Cancer Genome Atlas (TCGA) and the Cancer Cell Line Encyclopedia (CCLE) were two independent multi-omics datasets used to validate the findings. Functional molecular and pharmacologic perturbations in cell line-based experiments as well as pharmacologic perturbation experiments in experimental models were used to further validate the findings.
Given the growing body of evidence indicating that cells with a p-EMT phenotype play a crucial role in the progression of tumors into more advanced stages of disease, the findings of the study provide new information regarding additional therapeutic targets for this cancer. The study’s findings specifically suggest that catenin/CBP inhibition, which specifically targets more aggressive cells with elevated catenin/CBP activity, may be a promising treatment for head and neck cancer.
Although this study’s findings are limited to oral head and neck cancer, the authors believe that they may be applicable to other types of cancer, particularly those that originate in the mucosal tissues that line the respiratory, gastrointestinal, and genital tracts.
These discoveries seem online in the diary Translational Exploration.
More information: Eric R. Reed et al, β-catenin/CBP activation of mTORC1 signaling promotes partial epithelial-mesenchymal states in head and neck cancer, Translational Research (2023). DOI: 10.1016/j.trsl.2023.05.007